Radiology:SSc相关性ILD的评价,我们又近了一步
2021-07-26 shaosai MedSci原创
间质性肺疾病(ILD)是系统性硬化症(SSc)患者发病及死亡的主要原因。胸部高分辨率CT是检测ILD最可靠的影像学方法。初始ILD程度可预测疾病的进展和死亡率。
 间质性肺疾病(ILD)是系统性硬化症(SSc)患者发病及死亡的主要原因。胸部高分辨率CT是检测ILD最可靠的影像学方法。初始ILD程度可预测疾病的进展和死亡率。因此,CT在ILD的筛查和分期以及肺功能检查(PFTs)中起着重要作用。
间质性肺疾病(ILD)是系统性硬化症(SSc)患者发病及死亡的主要原因。胸部高分辨率CT是检测ILD最可靠的影像学方法。初始ILD程度可预测疾病的进展和死亡率。因此,CT在ILD的筛查和分期以及肺功能检查(PFTs)中起着重要作用。
对于疾病监测,PFT测量,尤其是按年龄和性别预测的用力肺活量是主要检测指标。根据美国胸科学会、欧洲呼吸学会、日本呼吸学会和拉丁美洲胸科学会的标准,在特发性肺纤维化的背景下,功能恶化定义为绝对用力肺活量相对下降10%或绝对一氧化碳弥散量(DLco)相对下降15%。但是,许多研究表明PFT的变化对疾病进展的监测效果过于片面,并建议将PFT测量与疾病进展的形态学评估相结合以提高准确性及特异性。在SSc患者中,CT扫描在监测ILD中的作用尚不明确。非特异性间质性肺炎是SSc相关性ILD的主要形式,其可从最初的炎症阶段发展为最终的肺纤维化。因此,ILD在CT扫描中的随访不仅需要比较疾病程度的改变,还需要评估与纤维化过程相关的肺萎陷情况。肺萎陷的评估更为复杂,需要在每个水平对CT图像进行并排比较。CT图像的弹性配准提供了一种定量手段,可在监测ILD进展过程中评估与恶化相关的肺萎陷程度。
近日,发表在Radiology杂志的一项研究开发了一种基于深度学习的方法,该方法可根据在随访期间获得的胸部CT图像的弹性配准检测肺萎陷情况,从而对SSc-ILD恶化做出相应的诊断,为临床提供了一个基于疾病进展的形态学变化的更准确且直观评价SSc-ILD的影像学手段。
本研究回顾性纳入2009年1月至2017年10月间评估的SSc患者,每位患者均在3个月内至少进行了两次平扫胸部CT扫描和肺功能检查(PFTs)。两名阅读者对CT扫描的形态学变化进行直观评估,并将其归类为ILD改善、稳定或恶化。对基线时和随访CT图像进行弹性配准,获得全肺变形图。将从变形图计算的雅可比行列式输入到基于深度学习的分类器中,以描述形态学和功能恶化。为此,该集合被随机分为训练集、验证集和测试集。用Spearman相关法评估平均雅可比矩阵值与PFT测量值变化之间的相关性。
本研究共纳入212例患者(中位年龄53岁;四分位数范围,45-62岁;177名女性):训练集138例(65%),验证集34例(16%),测试集40例(21%)。雅可比图显示,在视觉评估中发现恶化的患者肺实质萎陷发生于肺后基底部。该分类器检测到形态学和功能恶化的准确性分别为80%(40例患者中32例;95%置信区间[CI]: 64%,91%)和83%(40例患者中33例;95% CI: 67%,93%)。雅可比矩阵值与用力肺活量的变化(R = -0.38;95% CI: -0.25, -0.49; P < .001)和一氧化碳弥散量(R = -0.42;95% CI: -0.27, -0.54; P < .001)有相关性。

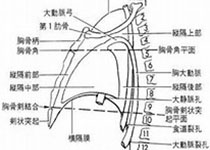
图 CT表现为进展和稳定的间质性肺病(ILD)患者的雅可比图。A,进展性ILD患者。随访53个月时胸部CT显示胸膜下网格样和磨玻璃密度灶增多。雅可比图显示这些区域的雅可比行列式对数增加,对应肺局部萎陷。该患者在功能和形态学上均表现为恶化,并通过深度学习模型正确识别。B,稳定的ILD患者。随访6个月时胸部CT显示舌段无磨玻璃密度灶或牵拉性支气管扩张的增加。雅可比图显示雅可比行列式对数接近于零,这与不存在局部肺萎陷相一致。使用深度学习模型正确识别功能和形态学的稳定。
本研究表明,结合深度学习分类器的CT扫描弹性配准可用于诊断系统性硬化症患者间质性肺疾病在形态学和功能上的恶化,为临床提供了一个更全面更准确地评估肺功能的影像学手段。
原文出处:
Guillaume Chassagnon,Maria Vakalopoulou,Alexis Régent,et al.Elastic Registration-driven Deep Learning for Longitudinal Assessment of Systemic Sclerosis Interstitial Lung Disease at CT.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ILD#
37
#相关性#
45
#评价#
37
#SSc#
34