Dermatol Ther:体外光疗治疗系统性硬化症的疗效与安全性
2022-07-28 sunshine MedSci原创
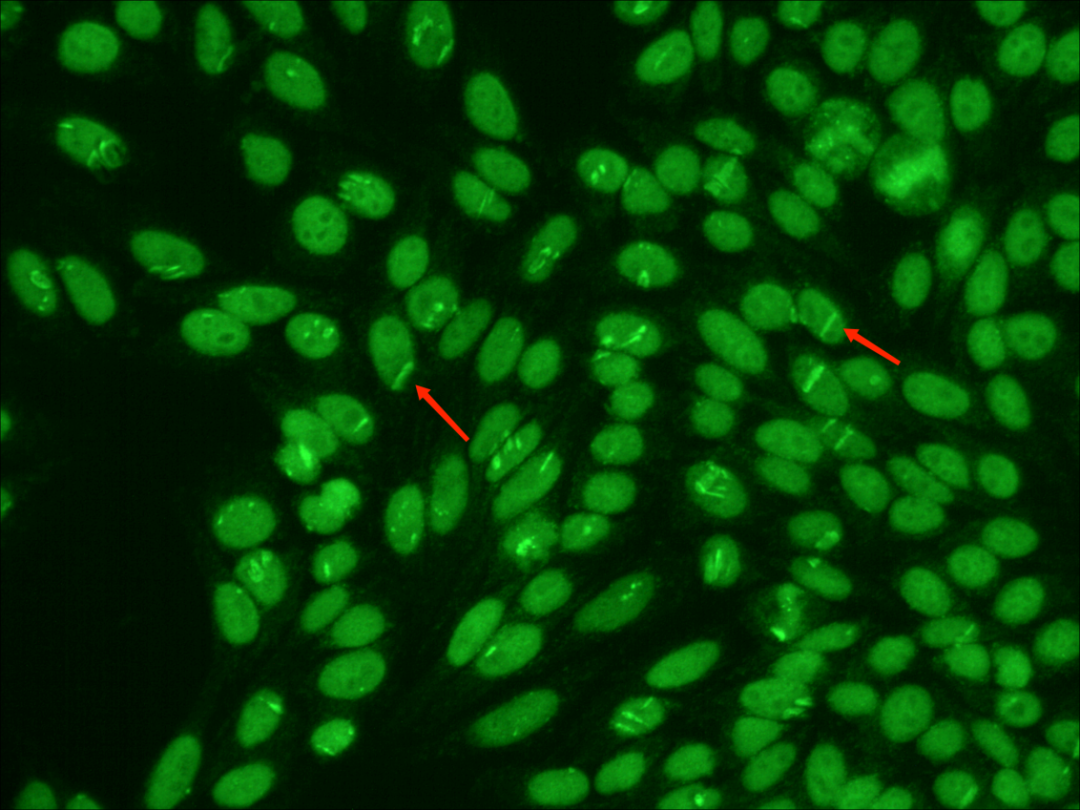
系统性硬化症(硬皮病)(SSc)是一种罕见的自身免疫性疾病,以胶原蛋白的过度产生为特征。体外光疗(ECP)涉及将外周血淋巴细胞反复暴露于紫外线A(UVA)辐射。
系统性硬化症(硬皮病)(SSc)是一种罕见的自身免疫性疾病,以胶原蛋白的过度产生为特征。体外光疗(photochemotherapy, phototherapy)(ECP)涉及将外周血淋巴细胞反复暴露于紫外线A(UVA)辐射。使用ECP治疗SSc患者的原因在于其假定的免疫调节作用,不过,关于ECP具体效果的严格数据是有限的,特别是在SSc患者中。近日,发表于Dermatol Ther的一项荟萃分析评估了体外光疗作为SSc患者治疗方式的效果。

研究人员在2022年3月13日搜索了CENTRAL和MEDLINE数据库,并纳入了关于诊断为SSc并接受ECP治疗的患者的随机临床试验(RCTs)。主要结果是皮肤评分的变化。采用多个观察者的独立提取和判断。使用反方差法和随机效应模型进行了荟萃分析;主要结果测量是皮肤评分的标准平均差异。
结果,研究人员共确定了三项相关的RCTs,包括162名随机(132名分析)接受ECP的患者,采用简单平行设计。这三项研究的汇总数据是无差异的。分析结果显示,与基线相比,标准平均差异为-0.11(95%置信区间为-0.45至0.23),P = 0.54,I2 = 0%。没有发现严重的治疗相关不良事件。
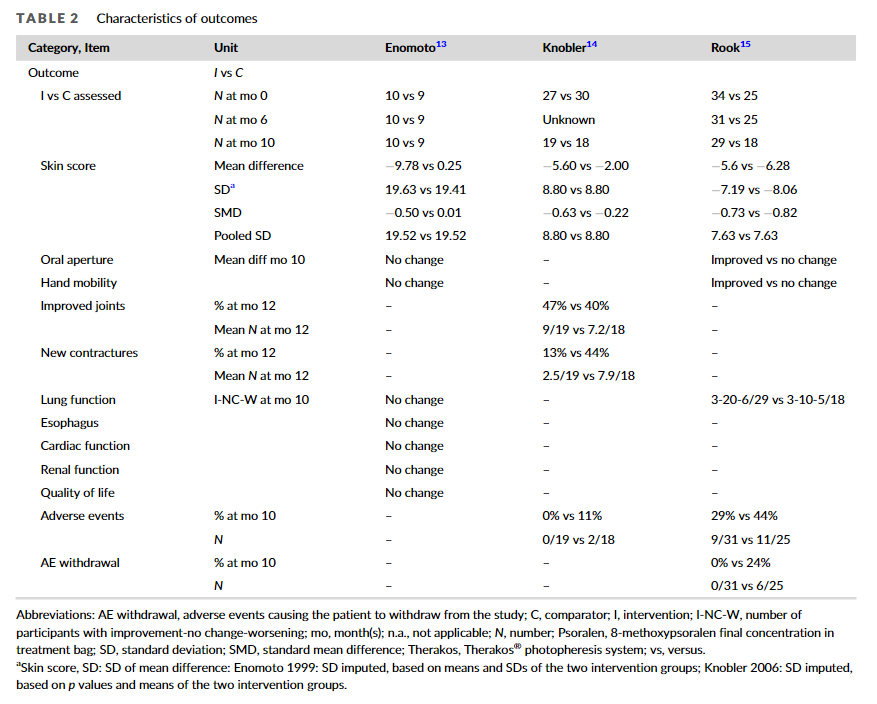
综上所述,该研究结果表明,与不治疗、假光疗或D-青霉胺相比,体外光疗对系统性硬化症患者皮肤评分的证据基础并不高,不足以支持其使用的优势效果。然而,ECP似乎是一种安全的治疗方法。未来的研究应明确报告内容,使用标准以达到高方法学质量,并使用经常应用的、适当的以患者为中心的结果,可以为医疗决策提供更好的参考。
原始出处:
Claudia Delbrück, et al., Extracorporeal photopheresis for systemic sclerosis: A meta-analysis of randomized clinical trials. Dermatol Ther. 2022 Jul;35(7):e15530. doi: 10.1111/dth.15530.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#系统性#
48
#光疗#
41
#硬化症#
34
#疗效与安全性#
45
#期刊论坛##学习#
62
不错的文章
48
#系统性硬化#
37