JAHA:心肌梗塞和心房颤动的危险因素、疾病发作和预后影响
2022-03-29 MedSci原创 MedSci原创
研究人员观察到心血管危险因素与两种疾病之间的不同关联,表明它们存在不同的病理生理途径。随后的MI和心房颤动诊断显著增加了死亡风险。
心肌梗死(MI)和心房颤动是常见的合并症。一种疾病的发作会显著增加另一种疾病的风险。已知MI病史是发生心房颤动的危险因素,与临床上明显的心力衰竭无关。
尽管MI和心房颤动是常见的合并症,并且具有共同的心血管危险因素,但这些危险因素与疾病发作、随后的疾病发病率和死亡率之间关联的方向和强度尚不完全明确。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在汇总的多变量Cox回归分析中,研究人员评估了108363名基线时无MI和心房颤动个体(中位年龄为46.0岁;48.2%为男性)疾病发作的时间关系,并确定了MI、心房颤动和全因死亡率的预测因子。6个基于欧洲人群的队列。
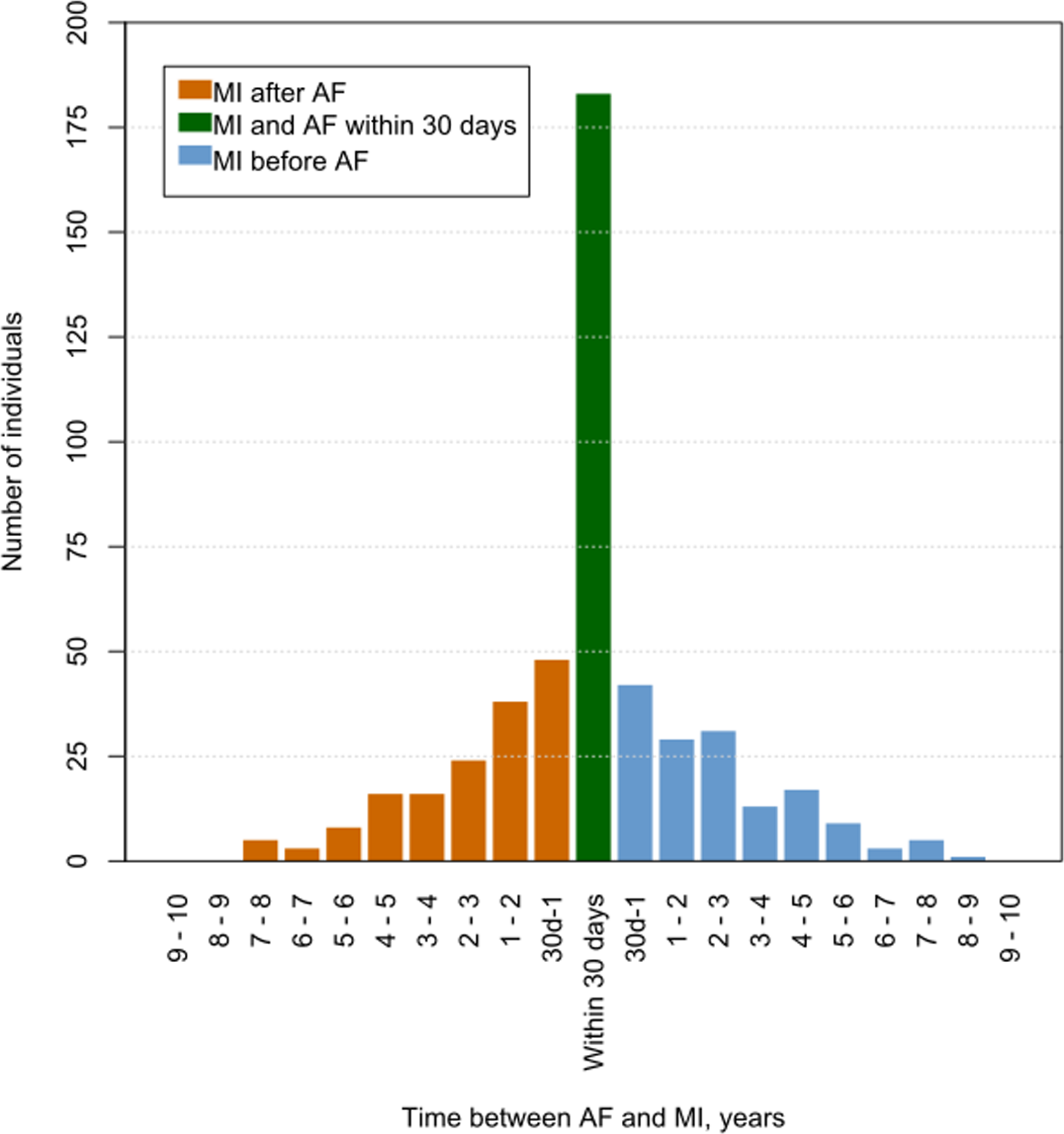
在最长10.0年的随访中,3558人(3.3%)被诊断为单纯心梗,1922人(1.8%)被诊断为心房颤动但没有心梗,491人(0.5%)被诊断为心梗合并房颤。与心房颤动相比,MI与性别、收缩压、抗高血压治疗和糖尿病的相关性似乎更强,而年龄和体重指数的增加表明心房颤动发生的风险更高。总胆固醇和每日吸烟与心梗事件显著相关,但与房颤无关。心血管危险因素的综合人群归因分数对于MI事件>70%,而对于心房颤动仅为27%。心房颤动后续MI(风险比[HR]为1.68;95%CI为1.03-2.74)和MI后的后续心房颤动(HR为1.75;95%CI为1.31-2.34)均显著增加患者的总体死亡风险。
由此可见,研究人员观察到心血管危险因素与两种疾病之间的不同关联,表明它们存在不同的病理生理途径。随后的MI和心房颤动诊断显著增加了死亡风险。
原始出处:
Stephan Camen,et al.Risk Factors, Subsequent Disease Onset, and Prognostic Impact of Myocardial Infarction and Atrial Fibrillation.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024299
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病发作#
39
学习
41
学习了
49
#AHA#
29
#心房#
29