血气分析如何判断动脉血、静脉血?
2018-05-02 黄驰 检验在线
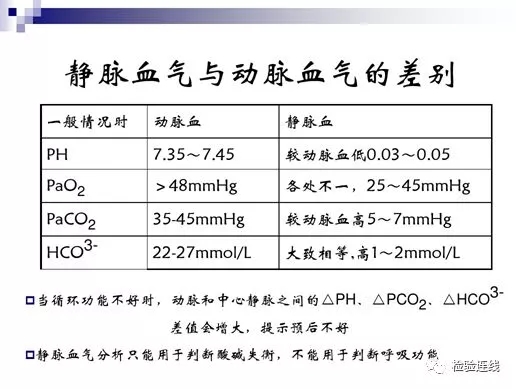
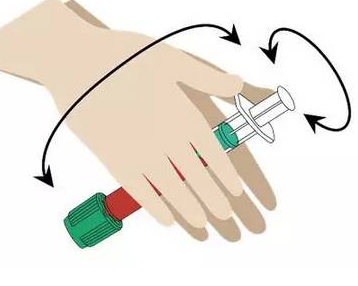
血气分析(BG)通过测定人体血液的H+浓度和溶解在血液中的气体(主要指CO2、O2),来了解人体呼吸功能与酸碱平衡状态的一种手段,它能直接反映肺换气功能及其酸碱平衡状态。采用的标本常为动脉血。临床上常碰到在穿刺过程中误取了静脉血标本,那么静脉血标本可以做血气分析吗?做出来的血气分析结果能反映病人的病情变化吗?能否从血气分析结果上辨别出血标本是静脉血还是动脉血呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉血#
0
#动脉血#
47
#静脉#
41
好文献.学习了
103
^_^^_^^_^
1