Eur Heart J:低死亡风险的肺栓塞患者右心室评估的临床意义
2021-06-28 MedSci原创 MedSci原创
通过超声心动图、计算机断层扫描或BNP/NT-proBNP和肌钙蛋白水平升高评估的RVD与低风险急性PE患者的短期死亡相关。
短期死亡风险较低的急性肺栓塞(PE)患者是家庭治疗或短期住院治疗的候选人群。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在明确右心室功能障碍(RVD)或肌钙蛋白升高是否比单独的临床模型更能提高对低风险患者的识别能力。
基于临床模型(肺栓塞严重程度指数、简化肺栓塞严重程度指数或Hestia),研究人员评估了低死亡风险的急性PE患者RVD或肌钙蛋白升高与短期死亡率之间关系研究中个体患者数据,并进行了荟萃分析。该研究的主要研究结局是短期死亡,定义为在院或30天内死亡。
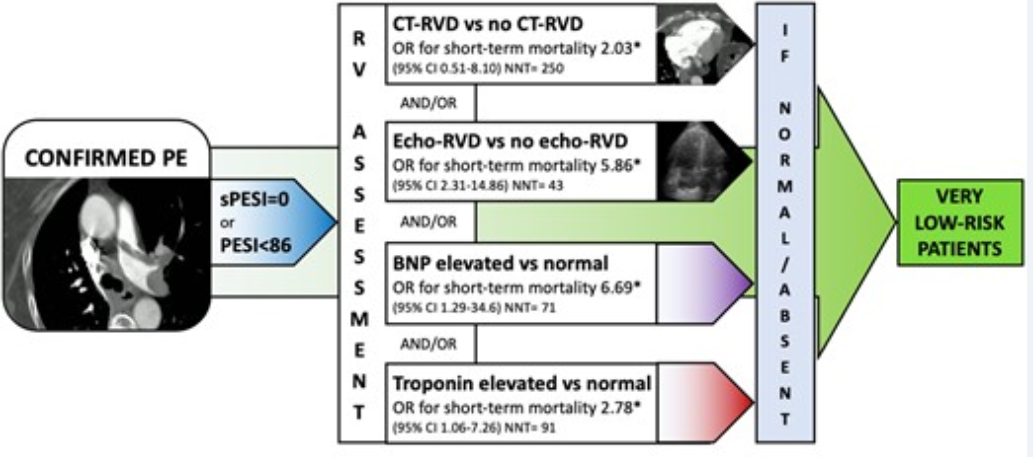
研究人员汇集了来自18项研究5010名低风险患者的个人数据。短期死亡率为0.7%[95%置信区间(CI)为0.4–1.3]。经超声心动图、计算机断层扫描或B型利钠肽(BNP)/BNP前体N末端(NT-proBNP)评估的RVD与短期死亡(1.5 vs. 0.3%;OR为4.81,95%CI为1.98–11.68)、3个月内死亡(1.6 vs. 0.4%;OR为4.03,95%CI为2.01–8.08)和PE相关死亡(1.1 vs. 0.04%;OR为22.9,95%CI为2.89–181)风险增加相关。肌钙蛋白升高与短期死亡(OR为2.78,95%CI为1.06–7.26)和3个月内死亡(OR为3.68,95%CI为1.75–7.74)相关。
由此可见,通过超声心动图、计算机断层扫描或BNP/NT-proBNP和肌钙蛋白水平升高评估的RVD与低风险急性PE患者的短期死亡相关。
原始出处:
Cecilia Becattini.et al.Right ventricle assessment in patients with pulmonary embolism at low risk for death based on clinical models: an individual patient data meta-analysis.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab329
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#死亡风险#
36
#ART#
38
#右心室#
41
#HEART#
42