Science Advances :苏佳灿/陈晓/陈啸飞研究团队揭示骨质疏松和骨折愈合治疗新靶点
2020-11-20 椰子 iNature
目前,全世界有超过2亿人罹患骨质疏松症,50岁以上人群中,骨量丢失导致老年人骨折风险及死亡率快速上升,每5名男性或3名女性中就有一人可能遭遇骨质疏松骨折。破骨细胞和成骨细胞共同维持骨代谢的平衡。
目前,全世界有超过2亿人罹患骨质疏松症,50岁以上人群中,骨量丢失导致老年人骨折风险及死亡率快速上升,每5名男性或3名女性中就有一人可能遭遇骨质疏松骨折。破骨细胞和成骨细胞共同维持骨代谢的平衡。抗骨吸收药物单纯抑制破骨细胞功能,阻碍了正常骨改建,对已经发生的严重骨质疏松效果不佳,存在影响骨折愈合的风险。近年来,促骨形成的靶点和药物越来越受到科研人员的重视。
2020年11月19日,海军军医大学苏佳灿/陈晓/陈啸飞研究团队在SCIENCE ADVANCES 杂志在线发表了题为“Targeting Actin-Bundling Protein L-Plastin as an Anabolic Therapyfor Bone Loss”的研究成果,该研究发现L-Plastin可以作为治疗骨质疏松和促进骨折愈合的潜在靶点。
L-Plastin(LPL)是肌动蛋白捆绑蛋白Plastin蛋白家族成员之一,其广泛表达于哺乳动物的髓系细胞中,如巨噬细胞,淋巴细胞,在细胞伪足形成,细胞迁移等过程中发挥非常重要的作用。单核细胞在巨噬细胞集落刺激因子(M-CSF)和核因子κB配体受体(RANKL)的诱导下形成破骨前体细胞,前体细胞融合形成成熟破骨细胞。破骨前体细胞可释放血小板生长因子BB(PDGF-BB)刺激CD31hiEmcnhi血管(H型血管)形成,促进骨形成。增加破骨前体细胞的数量能够促进H型血管形成,进而促进骨形成。
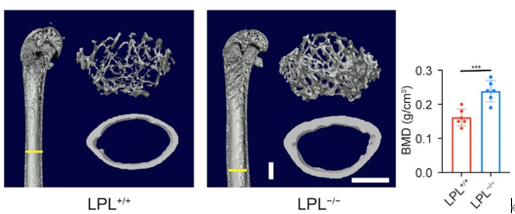
图1 .L-Plastin敲除小鼠骨量显着上升
研究团队构建了L-Plastin敲除小鼠,发现敲除小鼠骨骼中破骨前体细胞数量显着增加,H型血管生成增多,小鼠骨量显着增加,骨皮质厚度明显增加(图1)。进一步研究发现,L-Plastin参与调节破骨前体细胞丝状伪足的形成,影响破骨前体细胞的融合,调控成熟破骨细胞的形成,这一过程受PI3K-AKT-SP1信号通路的调节(图2)。通过制备新型L-Plastin共价生物色谱柱,运用研究团队自主设计的药物靶点MPTS共价固定化生物色谱-全二维液质联用分析系统(Acta Pharmaceutica Sinica B, 2020, 10(10): 1856-1865, IF 7.097),成功从中药黄芩中筛选得到L-Plastin特异阻断药物千层纸素A。研究团队发现千层纸素A能够减少小鼠绝经后骨质疏松骨量丢失,促进股骨干骨折愈合,同时申请了两项国家发明专利。
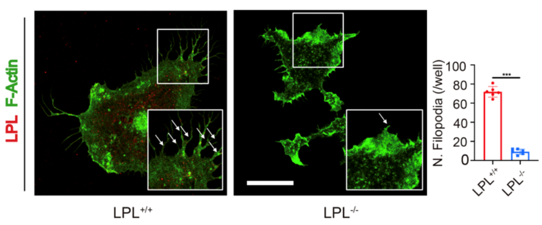
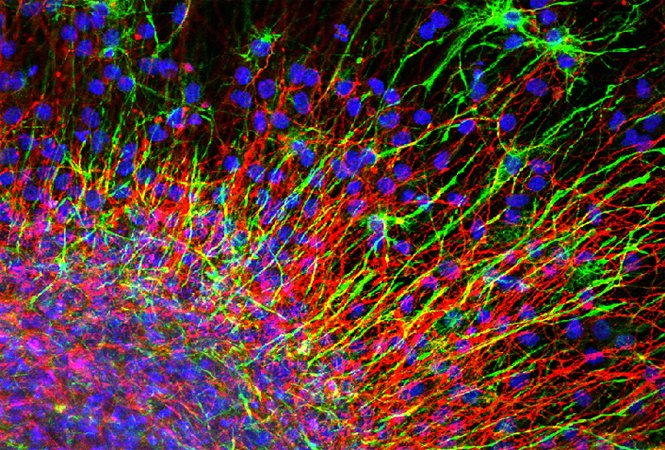
图2.L-Plastin调控破骨前体细胞丝状伪足形成
本项工作首次揭示了L-Plastin蛋白在破骨前体细胞融合中的作用,探究了其分子机制,阐明了L-Plastin蛋白与骨代谢过程之间的内在联系以及成骨破骨偶联的相关关系,丰富了人们对L-Plastin这一重要的肌动蛋白-捆绑蛋白功能的理解。同时,本研究筛选出L-Plastin靶向药物千层纸素A,验证了靶向L-Plastin在治疗骨丢失和促进骨折愈合中的作用,为今后药物研发提供了参考(图3)。
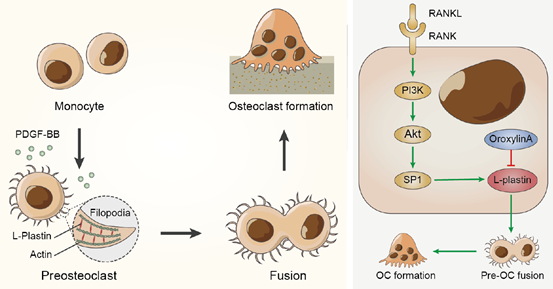
图3.L-Plastin调控破骨细胞融合机制
海军军医大学第一附属医院创伤骨科李啸群,医学影像科王立鹏,上海大学转化医学研究院黄标通,上海交通大学附属第九人民医院药剂科顾妍秋为本文的共同第一作者。海军军医大学第一附属医院创伤骨科苏佳灿、陈晓,海军军医大学药学院陈啸飞为本文的共同通讯作者。该研究得到了国家科技部重点研发计划(2018YFC2001500)、国家自然科学基金衰老领域重大研究计划重点项目(91749204)、国家自然科学基金面上项目(81771491、81871099)的资助。
原始出处:
Xiaoqun Li, Lipeng Wang, Biaotong Huang, et al.Targeting actin-bundling protein L-plastin as an anabolic therapy for bone loss.Sci Adv. 2020 Nov 18;6(47):eabb7135. doi: 10.1126/sciadv.abb7135. Print 2020 Nov.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨折愈合#
49
#苏佳灿#
40
#新靶点#
48
#SCIE#
52
#治疗新靶点#
58
#研究团队#
43
#骨质#
37
点赞!
87
学习了
91