EASD2018:又增实锤!糖尿病增加癌症风险
2018-10-04 国际糖尿病编辑部 国际糖尿病
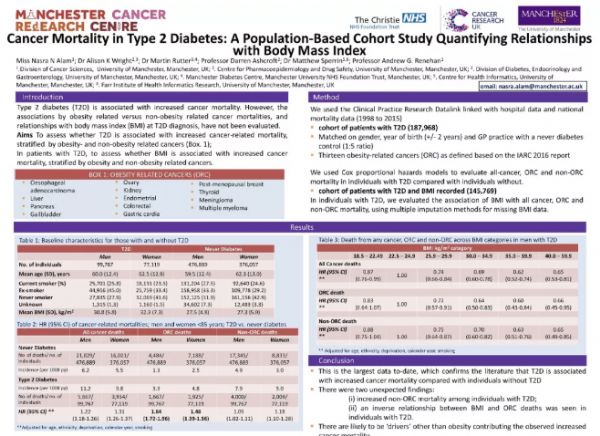
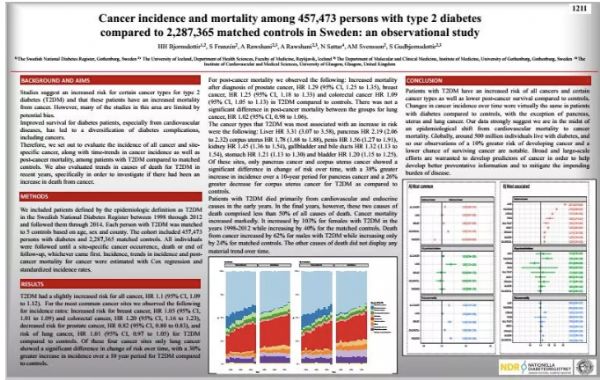
全球2型糖尿病患者数量已超4.15亿。既往研究显示2型糖尿病与癌症死亡率增加相关,肥胖亦可独立增加某些癌症的死亡风险。但是,上述风险增加是否与2型糖尿病直接相关?在第54届欧洲糖尿病研究协会年会(EASD 2018)上,两项糖尿病与癌症相关的研究公布(摘要号1117,摘要号1211),为糖尿病增加癌症风险再添证据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASD#
41
#EASD#
37
这个好,学习了,谢谢
58
需要仔细研究哦
53
不错的文章值得拥有,
60
学习了
52
学习了
55
好
29
了解一下,谢谢分享!
30
谢谢MedSci提供最新的资讯
19