Neurology:母语为汉语者的原发性进行性失语患者的书写困难表型
2022-05-16 Naomi MedSci原创
原发性进行性失语症(PPA)是一种以言语/语言障碍为最显著特征的神经退行性综合征。研究结果表明,正字法听写任务在汉语使用者中作为筛选工具和PPA分类指标的潜在作用,凸显语言多样性在PPA中的重要性。
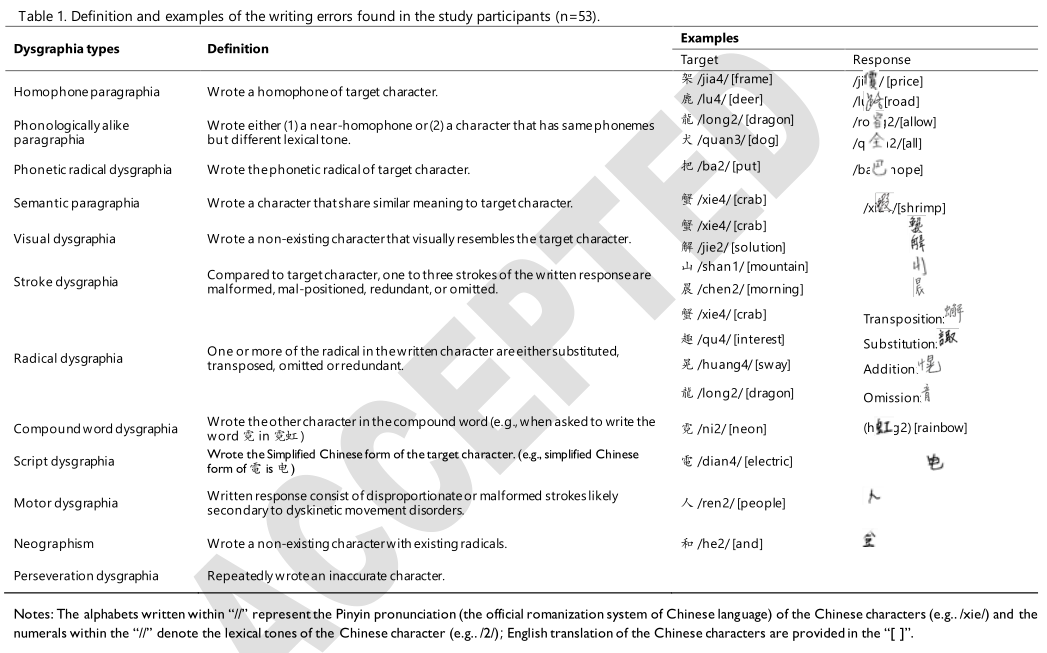
原发性进行性失语症(PPA)是一种以言语和/或语言障碍为最显著特征的神经退行性综合征。先前的研究表明,PPA患者存在书写障碍,不同PPA变异体的书写障碍表型各不相同。在说英语的PPA患者中,最常见的书写障碍错误是表层和语音书写障碍。表面书写障碍患者由于无法获得正字法全词形式(即词汇路径),通常基于字形-音素对应(即亚词汇途径)拼写单词;表面书写障碍通常会产生语音上看似合理的拼写错误,并且最常出现在语义变体PPA(SvPPA)个体中。相反,语音书写障碍被认为是语音路径的选择性损伤的产物,语音路径将音素与亚词汇水平上的相应拼写符号联系在一起。由于词汇路径保持不变,这些人保留了拼写现有规则和不规则单词的能力,但在拼写缺乏词汇表征的假词时遇到了困难。据报道,非流利/无语法PPA(NfvPPA)和对数变体PPA(LvPPA)都表现出语音书写困难,前者比可能的错误更容易出现语音上不可信的错误。另一种不常讨论的书写困难模式是由于拼写工作记忆恶化而发生的字形缓冲障碍。它通常显示与长度相关的字母省略、替换和添加。很少有病例报告描述了所有三种PPA变异体的字形缓冲障碍,尽管很少被描述为主要的书写困难类型。
迄今为止,关于PPA的文献大多涉及说英语的人。专门由讲英语的PPA个人产生的语言症状的跨语言有效性一直没有得到充分的理解,特别是在其他语言具有明显的语言特征的情况下。一个典型的例子是汉语的正字法系统。英语单词依赖字母表来构建单词并提供语音表示,而汉语采用由笔画(例如,一和丿)和部首(即,具有语义和/或语音信息的图形单位,例如,氵和工)来形成正字符号的象形文字。
中文标志通常指汉字,而现代汉语单词通常以两个或两个以上字符的复合词形式存在(例如,单词计算机“電腦”由字符电子“電”和大脑“腦”组成)。现代汉字主要由具有两个或两个以上部首的复合字组成,通常是一个语义部首和一个拼音部首,通常被称为义音复合字。然而,有相当一部分汉字要么是物体的图形描述(即,象形字,如表示太阳的象形字),要么是抽象的概念(即,表意字,如表示三的表意字),或者是没有音部首的复合字(例如,日)。“印”代表印章)。这些字符的正字法结构不携带语音信息;因此,它们的发音不能被次要地解码。即使是具有音部首的复合字,也只有1939%的义声复合字的读音与其音部首相似。因此,汉语通常被认为是弱形音素对应关系。此外,汉字通常具有丰富的同音字,平均每个字约有15个同音字。现代汉语通常采用双音节/两字词形式,以减少兼容单词的数量(例如,当“太阳”与“花”配对形成“向日葵”时,发音/ˈFlaʊ.ɚz/很容易辨认为“花”而不是“面粉”)。此外,现代汉字存在于16种以上的部首空间构形中,每个字的笔画数由1到64不等。
鉴于拼写结构的巨大差异,研究假设PPA患者的书写困难模式在使用英语和汉语的人中有所不同。事实上,少数描述中国PPA患者书写困难的案例报告揭示了在英语使用者中较少描述的拼写错误,特别是同音字错误、拼写相似错误和复合词错误的颠倒。虽然具有启发性,但这些案例报告主要提供了只涉及PPA变体之一的印象性发现。到目前为止,大多数初级进行性失语症(PPA)文献都是以英语使用者为基础的。自然,不同于英语的语言特征,如标志书写系统,没有得到充分的研究。
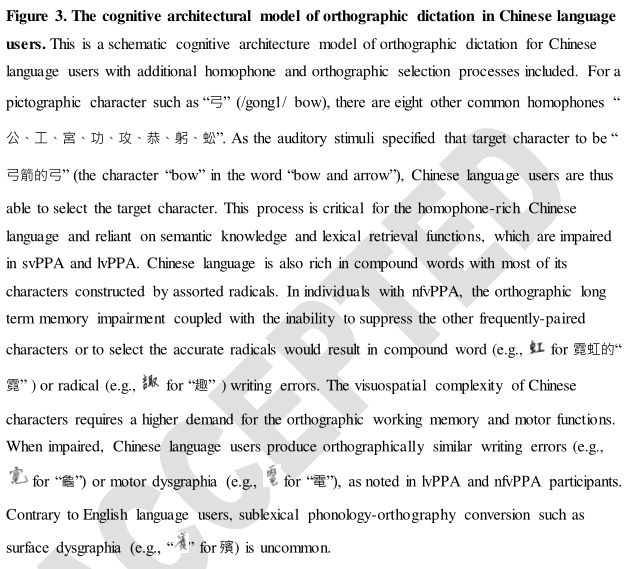
根据正字法加工的认知结构和三种PPA变体特有的神经解剖学变化,近日,一项发表在Neurology上的研究推测:(I)中国svPPA患者由于词汇-语义知识缺失而出现的语音似然错误的发生率更高;(Ii)由于视觉空间障碍,正字法相似错误在中国lvPPA患者中更为普遍;(Iii)nfvPPA中国人通常会出现继发于执行功能障碍的复合词错误。该研究的特点是用中文书写的PPA患者的书写困难表型,并探讨其在PPA变种分类中的诊断价值。
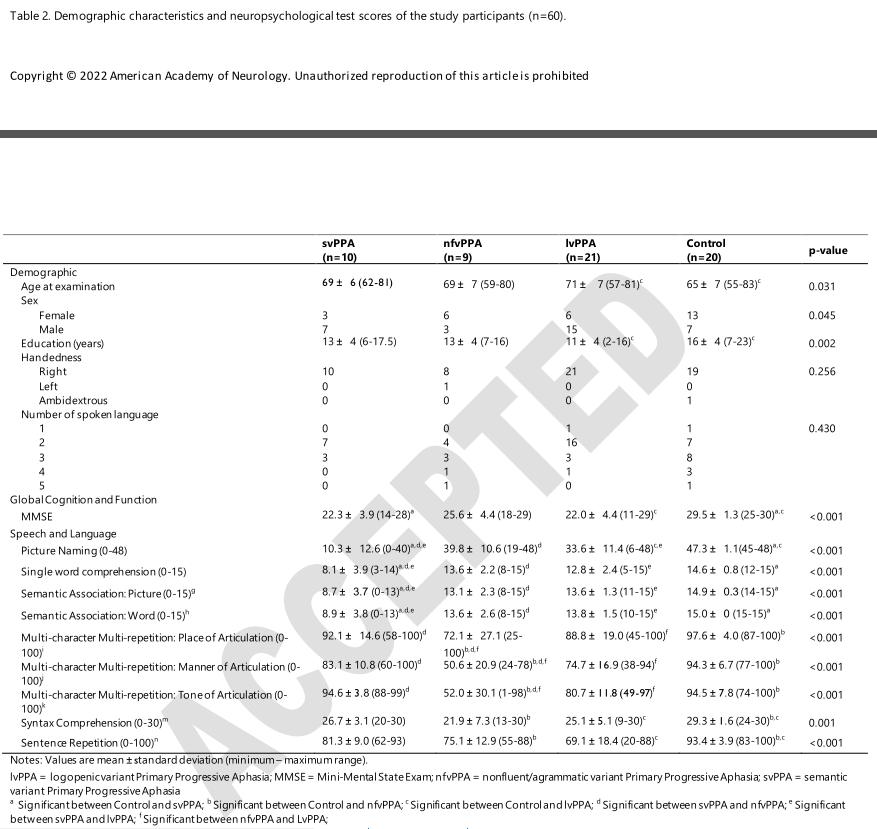
方法:本研究从旧金山、香港和台湾招募了40名PPA参与者和20名认知正常的参与者。我们使用PPA汉语评估(CLAP)60字正字法听写测试来测量听写准确性,并检查研究组中各种书写错误的发生情况。还进行了基于体素的形态计量学分析,以确定与听写准确性和书写错误发生率相关的灰质区域。
结果:
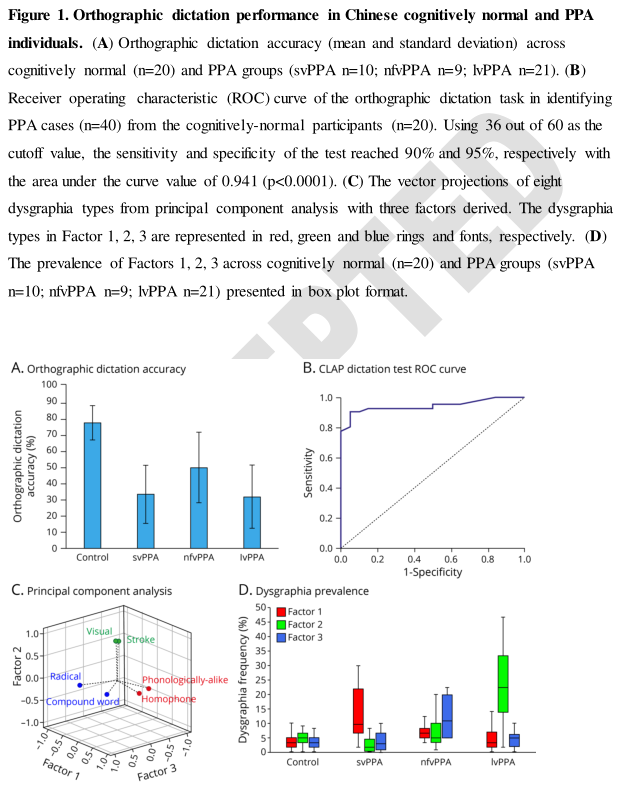
- 所有PPA组产生的准确书写反应都明显低于对照组,并且不同PPA变体之间的听写准确性没有显著差异。
- 在CLAP正字法听写任务中,以36分(满分60分)为切分,该测验识别中国PPA受试者与对照组的敏感度和特异度分别为90%和95%。
- 除字频效应外,svPPA和lvPPA组的同音字密度和笔划数也影响听写的准确性。
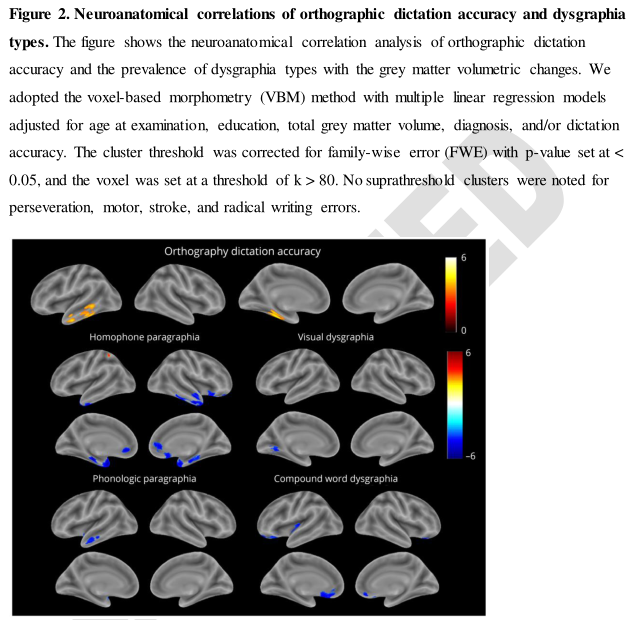
- 听写的准确性与左脑腹侧颞叶皮质的体积变化相关,这些区域被认为是拼写长期记忆的关键区域。
- 语义变异PPA的个体在词汇水平上经常出现语音似是而非的错误;对数变异PPA患者在视觉和笔划错误上具有更高的优势;不流利/无语法变异PPA患者通常表现为复合词和部首错误。
- 发音错误、视觉错误和复合词错误的发生率分别与双侧颞区、左侧颞枕区和双侧眶前回的皮质体积呈负相关。
讨论:
研究结果表明,正字法听写任务在汉语使用者中作为筛选工具和PPA分类指标的潜在作用。每个PPA变种都有特定的中文书写困难表型,这些表型与以前在英国PPA患者中报道的不同,突显了语言多样性在PPA中的重要性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#进行性#
31
#原发性#
51
#Neurol#
25
#失语#
41
吧
33
#表型#
34