Neuroradiology:RANO标准、对比增强和灌注MRI在评估胶质母细胞瘤进展的价值。
2017-09-19 shaosai MedSci原创
多形性胶质母细胞瘤简称为胶母细胞瘤,按Kernohan分类属星形细胞瘤3~4级。胶质母细胞瘤是最常见的脑胶质瘤之一,占胶质瘤的25%以上,也是最恶性的一种。男性多于女性,男女之比约为3:1。大多发生于成人,特别是30~50岁间。胶质母细胞瘤呈浸润性生长,病程迅速进展,手术切除后常很快复发。本研究旨在评价多形性胶质母细胞瘤(GBM)神经肿瘤反应评价标准关于Macdonald标准和对比增强(CE)体积
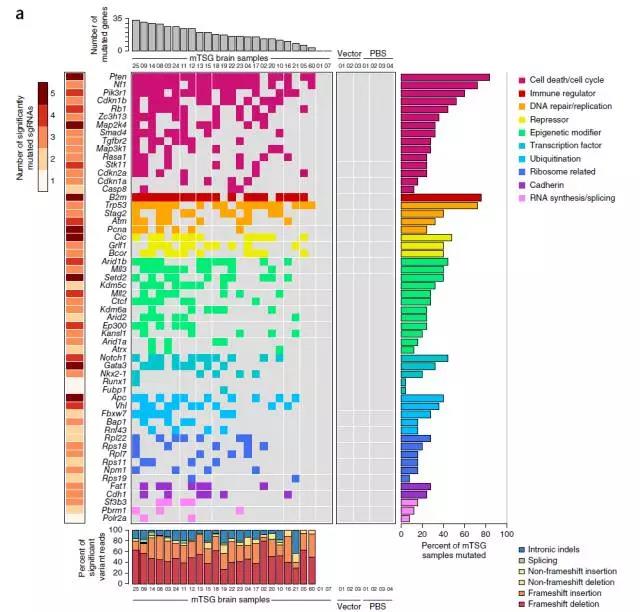
多形性胶质母细胞瘤简称为胶母细胞瘤,按Kernohan分类属星形细胞瘤3~4级。胶质母细胞瘤是最常见的脑胶质瘤之一,占胶质瘤的25%以上,也是最恶性的一种。男性多于女性,男女之比约为3:1。大多发生于成人,特别是30~50岁间。胶质母细胞瘤呈浸润性生长,病程迅速进展,手术切除后常很快复发。本研究旨在评价多形性胶质母细胞瘤(GBM)神经肿瘤反应评价标准关于Macdonald标准和对比增强(CE)体积变化的关系。并探究相对脑血流量(rCBV)的相对变化,并将结果发表在Neuroradiology上。本研究共纳入了自2006-2010年的43例患者,所有患者进行了手术切除,并行术后基于替莫唑胺的放化疗。回顾性分析MR图像。根据RANO标准的进展时间(TTPs),对比Macdonald标准和CE体积增加(CE-3D)间的差异,并评价rCBV第75%分位数(rCBV75)的百分比变化。在随访中位时间22.7个月之后,参照RANO标准、CE-3D和Macdonald标准,分别共有39、32、42例患者病变发生进展。中位TTPs分别为6.4、9.3和6.6个月。在RANO和CE-3D、RANO和Ma
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胶质母细胞#
31
#母细胞瘤#
30
#细胞瘤#
34
好好学习.谢谢分享!
67
学习了.谢谢分享
63
学习了新知识
70
学习了不少事情!
59