FDA即将批准液体活检技术Parsortix用于转移性乳腺癌
2020-10-22 Allan MedSci原创
液体活检公司ANGLE近日宣布,美国食品药品监督管理局(FDA)已对液体活检技术Parsortix用于转移性乳腺癌(MBC)患者的申请进行实质性审查。
液体活检公司ANGLE近日宣布,美国食品药品监督管理局(FDA)已对液体活检技术Parsortix用于转移性乳腺癌(MBC)患者的申请进行实质性审查。
9月28日,ANGLE表示已为其Parsortix系统提交了完整的II类FDA呈递文件,以寻求FDA批准用于MBC患者。提交之后,FDA已完成其行政复议,以确定提交的文件是否包含实质性复审所需的所有必要信息。
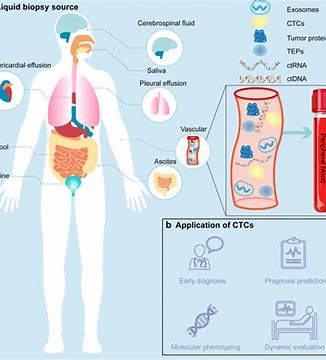
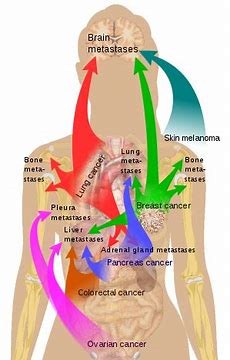
ANGLE的Parsortix系统使用细胞分离技术,该系统以可行的形式捕获所有类型的循环肿瘤细胞(CTC)以及CTC簇。CTC允许对DNA、RNA和蛋白质进行分析,从而可以对癌症进行全面了解,从而提供与组织活检类似的分析。此外,CTC分析是一种非侵入性过程,因此可以根据需要重复进行,这是重要的因素,因为癌症会随着时间的流逝而发生变化。
ANGLE的创始人兼首席执行官Andrew Newland表示:“我们相信,ANGLE拥有巨大的机会来确保获得FDA的批准,该平台可从患者血液中捕获并收集完整的循环肿瘤细胞用于后续分析,尤其是对于转移性乳腺癌”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#液体活检技术#
31
#活检#
28
#转移性#
25
学习了
99
期待更多的进步#乳腺癌#
128
学习学习
96
学习学习
95