DCR:术前营养评分可以作为 II 至 III 期结直肠癌患者总生存期和术后并发症的预测指标
2021-09-30 MedSci原创 MedSci原创
术前营养和炎症状态与术后患者的疾病结果息息相关,国际癌症控制联盟 (UICC) 在肿瘤淋巴结转移 (TNM) 分类中将营养状况和炎症评分列为食管癌、肝细胞癌的危险因素。
术前营养和炎症状态与术后患者的疾病结果息息相关,国际癌症控制联盟 (UICC) 在肿瘤淋巴结转移 (TNM) 分类中将营养状况和炎症评分列为食管癌、肝细胞癌和胰腺癌的患者的预后因素。然而,对于结直肠癌 (CRC)患者,只有年龄和种族是被列为宿主相关的预后因素。本研究的目的是评估营养和炎症评分对结直肠癌患者术后结局的预后意义。
这是一项在日本一家大型多学科三级癌症中心进行的回顾性研究。研究参与者是 2004 年-2012 年间在国家癌症中心医院接受根治性切除术的 1880 名II至III期结直肠癌患者。 两项营养评分问卷(预后营养指数和控制营养状况评分)和 4项炎症评分(改良格拉斯哥预后评分)、中性粒细胞/淋巴细胞比、血小板/淋巴细胞比和 C 反应蛋白/白蛋白比)被研究人员分别测量和统计。主要观察指标是营养评分和炎症评分与总生存期和术后并发症的相关性。
通过多变量分析调整临床和病理关键因素后,2个营养评分(预后营养指数和控制营养状况评分)和2个炎症评分(中性粒细胞/淋巴细胞比和C反应蛋白/白蛋白比)是总生存期的独立预后因素. 在判别能力方面,时间依赖性受试者操作特征曲线和 Harrell 一致性指数显示,预后营养指数和控制营养状况评分用于预测总生存期的能力优于4项炎症评分。多变量逻辑回归分析也显示预后营养指数、控制营养状况评分和 C 反应蛋白/白蛋白比率是术后并发症的独立预测因素。
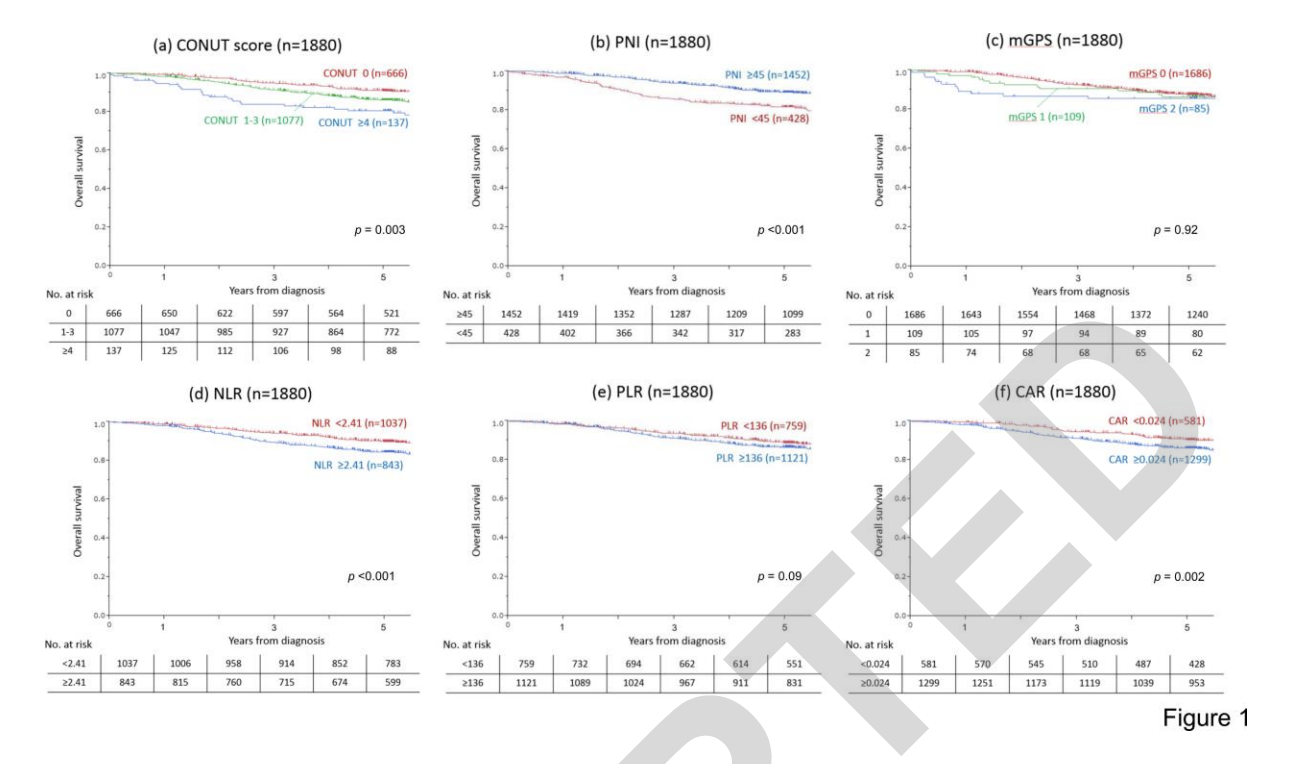
本项研究证实术前营养评分是 II 期和 III 期结直肠癌患者总生存期和术后并发症的预后因素。
原始出处:
Ahiko, Yuka. Et al. Preoperative Nutritional Scores as Host-Related Prognostic Factors for Both Overall Survival and Postoperative Complications in Patients With Stage II to III Colorectal Cancer.Diseases of the Colon & Rectum.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#III#
53
#并发#
45
#生存期#
43
#预测指标#
43
#结直肠#
41
#总生存期#
0