Hypertension:高血压患者突发心脏病死亡情况分析
2019-03-04 xing.T 网络
由此可见,在没有明确心血管疾病的高血压患者中,年龄、糖尿病、心电图左心室肥厚和24小时动态脉压是长期SCD的独立预后指标。
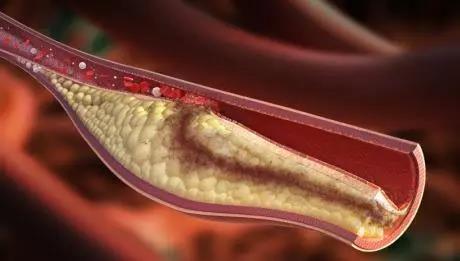
在无明确心血管疾病的高血压患者中,心源性猝死(SCD)的预测因素仍未确定。
近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员对3242名最初未接受过治疗的高血压患者平均随访了10.3年,他们在入组时没有冠状动脉或脑血管疾病的证据。所有患者均接受了完整的临床检查,包括心电图和24小时动态血压监测。
入组时,患者的平均年龄为50.0岁,45%为女性,6.1%为2型糖尿病患者。平均诊室血压为154/96 mmHg,平均24小时动态血压为136/86 mmHg。心电图左心室肥厚的患病率为13.9%。在随访期间,33名患者发生SCD,发生率为每100名患者每年0.10人(95%CI为0.07-0.14)。在没有和有心电图左心室肥大的患者队列中,SCD的发生率分别为每100名患者每年0.07和0.30人(P<0.01)。在一个多变量Cox模型中,左心室肥大在调整年龄(P<0.0001)、性别(P=0.019)、糖尿病(P<0.0001)和24小时动态脉压(P=0.036)后几乎使SCD的风险增加三倍(校正风险比为2.99; 95%CI为1.47-6.09; P=0.002)。对于24小时动态脉压每增加10mmHg,SCD的风险增加35%。受试者工作特性曲线下的时间依赖性面积为0.85(95%CI为0.74-0.96)。
由此可见,在没有明确心血管疾病的高血压患者中,年龄、糖尿病、心电图左心室肥厚和24小时动态脉压是长期SCD的独立预后指标。
原始出处:
Paolo Verdecchia.et al.Sudden Cardiac Death in Hypertensive Patients.Hypertension.2019.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.119.12684
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TENS#
0
#PE#
30
#心脏病死亡#
35
#高血压患者#
34
#Hypertension#
31