J Thorac Oncol: 经治晚期NSCLC使用Atezolizumab单药治疗进展后再联合贝伐珠单抗治疗的疗效
2022-05-23 yd2015 网络
研究表明,经治晚期NSCLC使用Atezolizumab单药治疗进展后再联合贝伐珠单抗治疗具有良好的抗肿瘤活性和耐受性。
近期,Journal of Thoracic Oncology杂志上发表了一项II期临床研究结果,主要是评估经治晚期NSCLC使用Atezolizumab单药治疗进展后再联合贝伐珠单抗治疗的疗效。

该研究为两阶段的II期临床研究,纳入患者为至少接受一线铂类为基础化疗进展的NSCLC,且EGFR/ALK阴性。第一阶段为接受Atezolizumab单药1200 mg/3周治疗直至影像学进展;第二阶段为进展后再联合贝伐珠单抗15 mg/kg/3周。主要终点为第二阶段的疾病控制率(DCR)。
阶段I和阶段II分别纳入42名和24名患者。平均年龄为66岁。大多数为男性(59.5%),E CO=1 (97.6%),有吸烟史(54.8%)。脑转移发生率为33.3%。大多数患者为非鳞状组织亚型(92.9%),PDL1表达阴性(71.4%)。
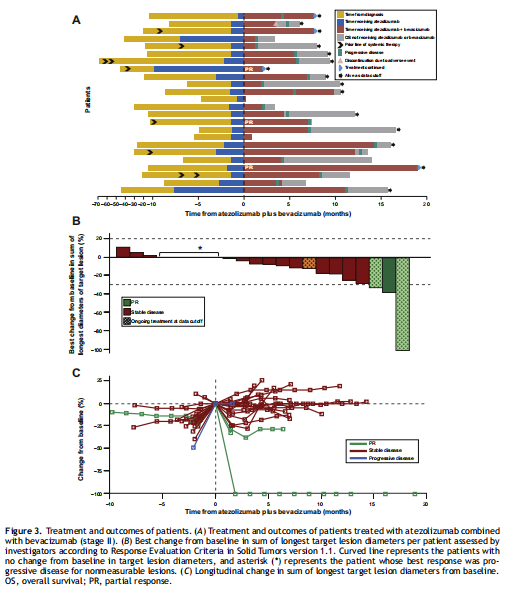
中位随访时间为14.0个月(95% CI: 6.1 21.9)。阶段I的42例患者的中位治疗时间为1.4 (95% CI: 1.4-1.4)个月,阶段II的24例患者的中位治疗时间为5.9 (95% CI: 1.9-9.9)个月。在第一次治疗评估之前,阶段I和阶段II分别有3名和2名死于疾病进展(n=4)或AEs (n=1,心脏骤停)。
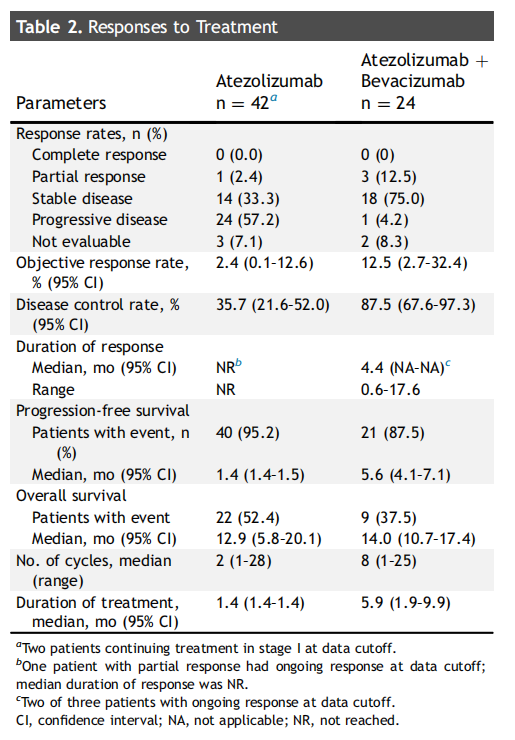
该研究达到研究终点,第二阶段的疾病控制率(DCR)为87.5% (95% CI: 67.6-97.3, 21 / 24),其中3例患者获得部分缓解,18例病情稳定。第二阶段患者的中位PFS和OS 分别为5.6(95%CI: 4.1 - 7.1)和14.0(95% CI:10.7—17.4)个月。12个月的OS率63%。相比之下,第一阶段1例患者获得部分缓解,14例患者获得病情稳定,DCR为35.7% (95% CI: 21.6 52.0, 15 / 42),中位PFS为1.4个月(95% CI: 1.4 1.5)。

在纳入第二阶段的患者中,41.7%(95% CI: 22.1 63.4, 10 / 24)实现了持久的临床受益(DCB),定义为疾病获得持续6个月以上的缓解或稳定。
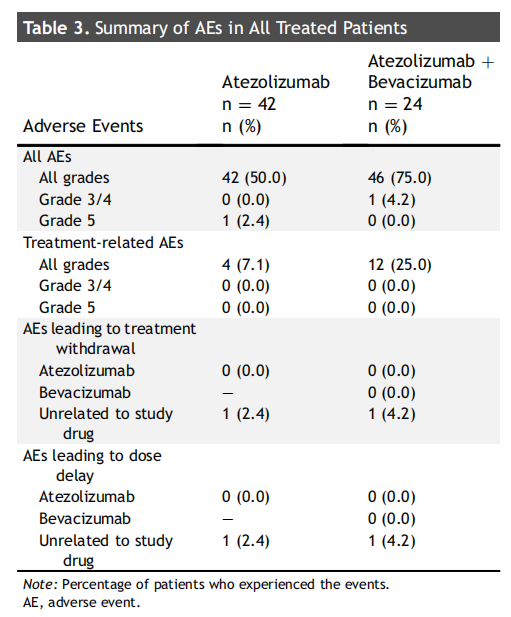
第二阶段患者中25%患者发生治疗相关不良事件,但均为1级或2级。
综上,研究表明,经治晚期NSCLC使用Atezolizumab单药治疗进展后再联合贝伐珠单抗治疗具有良好的抗肿瘤活性和耐受性。
原始出处:
Lee J, Koh J, Kim HK, Hong S, Kim K, Park S, Jung HA, Sun JM, Lee SH, Ahn JS, Park K, Ahn MJ. Bevacizumab Plus Atezolizumab After Progression on Atezolizumab Monotherapy in Pretreated Patients With NSCLC: An Open-Label, Two-Stage, Phase 2 Trial. J Thorac Oncol. 2022 Apr 12:S1556-0864(22)00193-9. doi: 10.1016/j.jtho.2022.04.001. Epub ahead of print. PMID: 35427805.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#单药治疗#
47
#Oncol#
39
#THORAC#
43
#贝伐珠#
34
#mAb#
39
#晚期NSCLC#
33
#贝伐#
34
JTO上文章都很好,谢谢梅斯及时上新
33