JGH:胸腺素 β10 (TMSB10) 可作为胃癌侵袭性的潜在预后预测生物标志物
2021-06-23 MedSci原创 MedSci原创
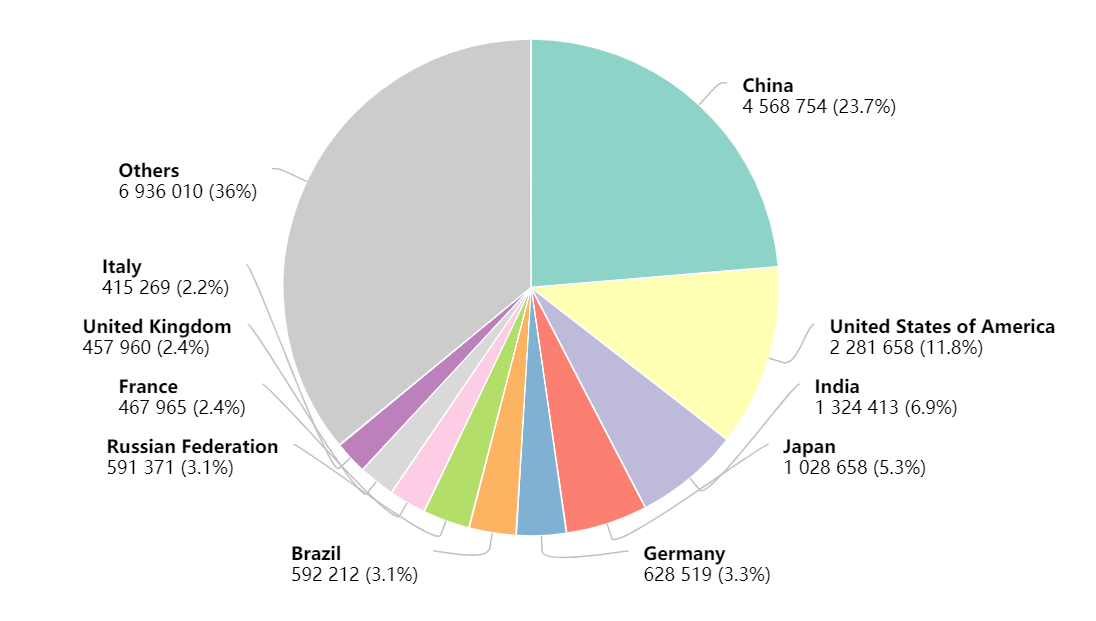
胃癌 (GC) 是中国发病率第二高的恶性肿瘤,并且仍然是发展中国家癌症相关死亡的主要原因之一。
胃癌 (GC) 是中国发病率第二高的恶性肿瘤,并且仍然是发展中国家癌症相关死亡的主要原因之一。 尽管近年来,胃癌患者的发病率和死亡率呈下降趋势,但GC的早期诊断率低,5年生存率仍低于20%,中位生存率大约 10 个月。 因此, 迫切需要胃癌的预后生物标志来改善GC 的早期诊断和远期预后。胸腺素β10 (TMSB10) 最初是从胸腺中发现的,它在许多癌症的发展中起着关键作用。然而,尚未了解 TMSB10 是否参与了GC的发病。

为了确定TMSB10在人胃癌组织中的表达情况,并说明其是否与胃癌患者的临床病理特征和预后相关。研究人员通过体外和离体GC 细胞的 TMSB10 敲低/过表达对其在调节肿瘤生长、侵袭和血管生成中的作用和潜在机制进行了研究。
研究结果显示在 GC 细胞和组织中TMSB10 蛋白表达的显着过表达,这与晚期肿瘤分期和 GC 患者的淋巴结 (LN) 转移有关。此外,预后分析表明,具有高 TMSB10 表达的 GC 患者的生存期显着缩短,并且TMSB10是预测 GC 患者总体生存率差的重要因素。此外,TMSB10 过表达会促进GC细胞的增殖过程和血管生成的速度。

图:胸腺素 β10 (TMSB10)在体内分布
本项研究的结果证实TMSB10 可能有望成为诊断 GC 的潜在预后预测生物标志物和潜在的治疗靶点。
原始出处:
ZhenKun Yan. Et al. TMSB10 can serve as a potential prognosis prediction biomarker and promotes the invasion and angiogenesis of gastric cancer. J Gastroenterology H.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胸腺#
51
#TMS#
37
#标志物#
35
#侵袭性#
35
#生物标志#
24
#生物标志#
37
学习了
60