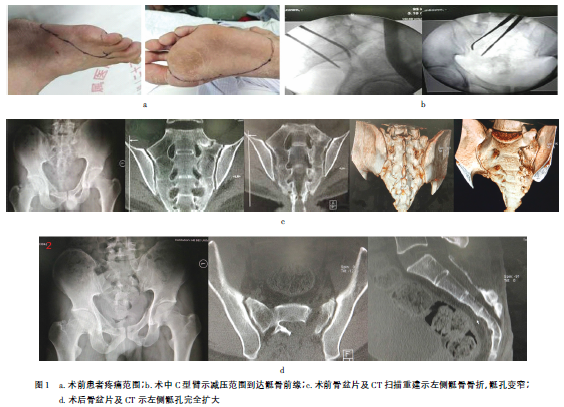
陈旧性骶骨骨折合并骶神经损伤术后1例
2018-11-23 周晓哲 创伤外科杂志
骶骨骨折在骨盆骨折中占14.0%~30.4%,其中15%~69%合并有神经损伤。由于患者就诊时多合并休克及其他脏器损伤,因此骶骨骨折往往得不到及时诊治。有些骶骨骨折早期并无神经症状,但是在非手术治疗过程中患者不能严格卧床或由于骨痂的形成,骶神经孔逐渐变窄,造成神经受压迫,从而导致神经症状的发生。因此骶骨骨折是否需要早期手术探查减压、手术入路、减压后固定方式等目前仍存在争议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#损伤#
36
#陈旧性#
29
#神经损伤#
37
学习了
57