JAMA Neurol:糖酵解增强型α-1受体阻滞剂与帕金森病发病风险的关系
2021-02-19 MedSci原创 MedSci原创
使用糖酵解增强药物,如特拉唑嗪、多沙唑嗪和阿福唑嗪,与使用坦索罗辛(一种针对类似适应症但不能增强糖酵解的药物)相比,是否与降低帕金森病风险相关?
帕金森病(PD)是一种常见的神经退行性疾病。预防或延迟PD发展是一个关键的临床上还未满足的需求。最近在动物模型和人类临床数据库中发现特拉唑嗪和与其密切相关的药物可以增强糖酵解,从而减少帕金森病进展。为了确定特拉唑嗪、多沙唑嗪和阿夫唑嗪是否与帕金森病发生风险的降低是否相关,有研究者使用来自美国和丹麦两个大型行政卫生保健数据库的数据对这一假设进行了检验。该研究结果近日发表在JAMA Neurology杂志上。
这项队列研究使用了来自丹麦全国卫生注册中心(包括丹麦国家处方注册中心、丹麦国家患者注册中心和丹麦民事注册系统)的主动对照和倾向评分匹配数据,以及1996年1月至2017年12月,以及2001年1月至2017年12月来自Truven Health Analytics MarketScan数据库的数据。在丹麦,该数据库包括所有居民,而Truven数据库是美国各地保险索赔的汇编。分析了2019年2月至2020年7月的数据。
研究者对使用特拉唑嗪/多沙唑嗪/阿福唑嗪vs坦索罗辛的患者还进行了额外的剂量反应分析。主要结局及测量:曾经使用过特拉唑嗪/多沙唑嗪/阿呋唑嗪或坦索罗辛的患者之间通过诊断或使用PD特异性药物确定的PD发病风险差异。
研究结果显示,在丹麦登记处确定了52365对特拉唑嗪/多沙唑嗪/阿法唑嗪和坦索罗辛使用者的倾向性得分配对队列,其中均为男性,平均(SD)年龄为67.9(10.4)岁;在Truven数据库中确定了94883对倾向性得分配对,其中均为男性,平均(SD)年龄为63.8岁(11.1)年。丹麦队列中使用特拉唑嗪/多沙唑嗪/阿法唑嗪的患者发生PD的危险比(HR)为0.88(95%CI,0.81-0.98),而Truven队列中的患者HR为0.63(95%CI,0.58-0.69)。在丹麦队列和Truven队列中,短期、中期和长期使用特拉唑嗪/多沙唑嗪/阿法唑嗪使用者的HR降低与剂量反应相关。
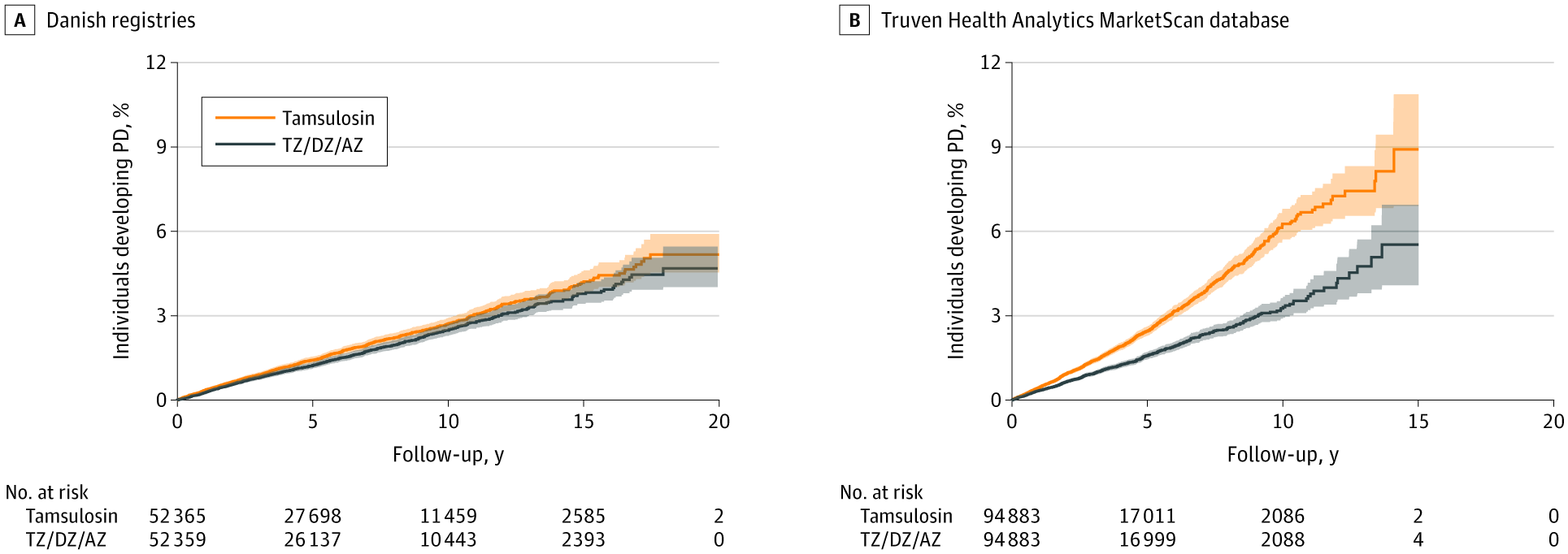
丹麦和Truven队列中帕金森病(PD)的累积发病率
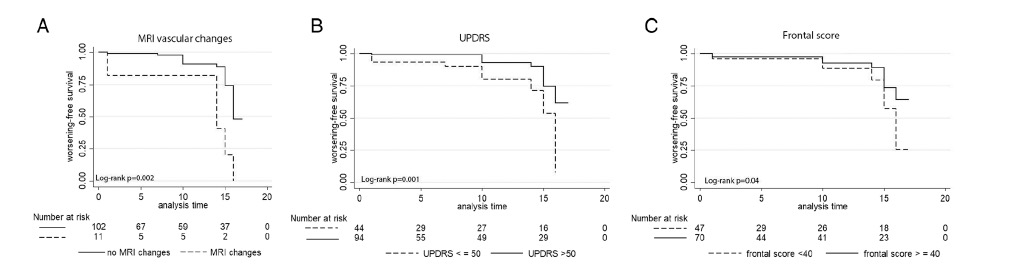
这些结果表明,服用TZ/DZ/AZ(特拉唑嗪/多沙唑嗪/阿法唑嗪)的男性发生PD的危险比服用坦索罗辛的男性低12%至37%。与使用坦索罗辛在相同时间内相比,长时间使用TZ/DZ/AZ与观察到的危害更多的减少相关。并且TZ/DZ/AZ与PD患者与疾病进展缓慢和并发症减少相关。
TZ/DZ/AZ的这些效应的潜在分子机制已被早期的研究所证实。TZ/DZ/AZ增强PGK1活性,从而增加糖酵解和细胞ATP水平。这些变化可能至少通过两种方式阻止PD神经退行性变。首先,PD表现出能量代谢的缺陷,表现为与衰老相关的ATP和能量代谢的下降、线粒体功能的遗传缺陷和线粒体功能的毒素抑制。通过增强糖酵解和增加ATP水平,TZ/DZ/AZ可以抵消这些缺陷。第二,假设α-synuclein的聚集体诱导PD的神经退行性变。TZ/DZ/AZ升高ATP,ATP是一种可能阻止聚集体形成和溶解先前形成的聚集体的水解酶。因此,如果假设的α-synuclein和神经退行性变的关系是正确的,TZ/DZ/AZ可能通过预防PD而降低PD的风险聚集性神经退行性变。然而,对这一假设机制的评估超出了本研究的范围。这些机制和其他机制的结合也是可能的,包括ATP依赖的解聚物和减少细胞凋亡的伴侣。
因此,需要进行进一步的研究,以确定特定的患者子集是否更有可能从治疗中获益。不管这些考虑,未来的工作,特别是以随机试验的形式,需要充分解决与TZ/DZ/AZ的因果关系有关的问题。
参考文献:Simmering JE, Welsh MJ, Liu L, Narayanan NS, Pottegård A. Association of Glycolysis-Enhancing α-1 Blockers With Risk of Developing Parkinson Disease. JAMA Neurol. Published online February 01, 2021. doi:10.1001/jamaneurol.2020.5157
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#受体阻滞剂#
49
#Neurol#
69
#风险的关系#
44
好方向
103
#阻滞剂#
43
#糖酵解#
41
学习了
77
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
61