Circulation:主动脉内球囊反搏在心源性休克并发急性心肌梗死患者中的作用
2018-11-12 xing.T MedSci原创
由此可见,IABP对6年长期随访的全因死亡率没有影响。死亡率仍然非常高,尽管当前采用血运重建治疗,仍有三分之二的心源性休克患者死亡。
尽管IABP-SHOCK II试验(主动脉球囊在心源性休克中作用试验II)得出的中性结果随后在国际指南中有所降级,但主动脉球囊反搏(IABP)在心源性休克中的作用仍然是一个激烈争论的话题。到目前为止,缺乏关于IABP对心源性休克并发急性心肌梗死患者的长期临床结局影响的随机数据。此外,实践治疗中心源性休克患者的一般长期结局只有有限的证据可用。
近日,心血管领域权威杂志Circulation上发表了一篇研究文章,IABP-SHOCK II试验是一项多中心、随机、开放分组试验。在2009年至2012年期间,600名心源性休克并发急性心肌梗死的患者接受了早期血运重建,随机分为IABP组和对照组。
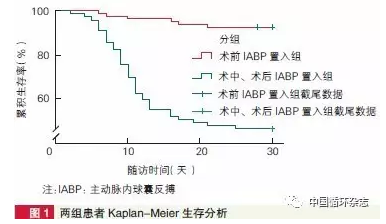
自随机化后,长期随访时间为6.2年(四分位间距5.6-6.7)。研究人员对600名患者中的591名患者(98.5%)进行了随访。IABP组和对照组的死亡率没有差异(66.3% vs. 67.0%;相对风险为0.99; 95%CI为0.88-1.11; P=0.98)。复发性心肌梗死、卒中、再次血运重建或因心脏原因再入院在两组间也没有差异(所有P>0.05)。通过EuroQol 5D调查问卷和纽约心功能等级评估的幸存者的生活质量在各组之间没有差异。
由此可见,IABP对6年长期随访的全因死亡率没有影响。死亡率仍然非常高,尽管当前采用血运重建治疗,仍有三分之二的心源性休克患者死亡。
原始出处:
Holger Thiele,et al.Intraaortic Balloon Pump in Cardiogenic Shock Complicating Acute Myocardial Infarction: Long-Term 6-Year Outcome of the Randomized IABP-SHOCK II Trial. Circulation. 2018. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.038201
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心源性休克#
26
#球囊#
32
#主动脉#
23
#心源性#
37
#并发#
36
好
54
好
64