Jpn J Nurs Sci:与BD Venflon™相比,BD Insyte™ Autoguard™ BC winge导管静脉炎的发生率较低
2020-11-15 MedSci原创 MedSci原创
本研究旨在确定两类导管材料(维亚隆生物材料和特氟隆)对外周静脉导管(PIVC)置管的疼痛强度、停留时间和静脉炎评分的影响,研究结果已在线发表于pn J Nurs Sci。
本研究旨在确定两类导管材料(维亚隆生物材料和特氟隆)对外周静脉导管(PIVC)置管的疼痛强度、停留时间和静脉炎评分的影响,研究结果已在线发表于pn J Nurs Sci。
将参与者(N = 208)随机分配到vialon生物材料组(n = 104)和特氟隆组(n = 104)。PIVC置管后,评估疼痛强度和静脉炎评分。测定导管滞留平均时间。
结果显示,插入PIVC后,两组患者的疼痛强度评分相似,疼痛评分之间无差异(P≥.050)。与特氟龙导管组(4.10±0.92天)相比,vialon生物材料导管组的导管滞留平均时间(4.72±1.20天)明显延长(p≤.001)。经测定,vialon生物材料导管组和特氟龙导管组分别有16.3%和53.8%的导管因静脉炎而被拔除。两组在静脉炎发展评分方面存在统计学差异(P≤.001)。
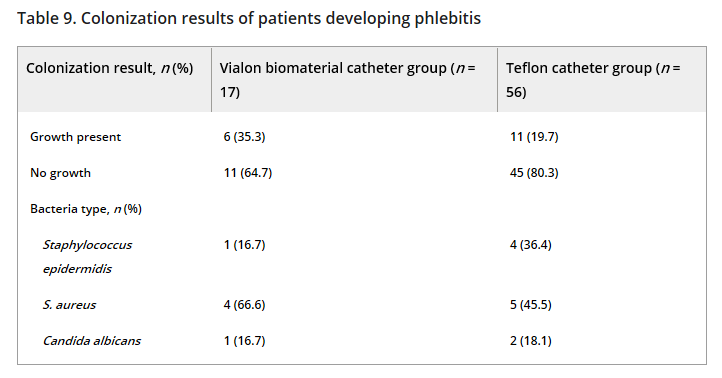
综上所述,该研究结果表明,vialon生物材料导管(BD Insyte™ Autoguard™ BC winged)比特氟隆导管(BD Venflon™)表现出更长的PIVC滞留时间、更低的静脉炎发生率和静脉炎评分。
原始出处:
Betül Kuş, Funda Büyükyılmaz, et al., Effectiveness of vialon biomaterial versus teflon catheters for peripheral intravenous placement: A randomized clinical trial. Jpn J Nurs Sci. 2020 Jul;17(3):e12328. doi: 10.1111/jjns.12328.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
28
#发生率#
21
#静脉炎#
38
#NFL#
28
学习
78