Blood:小分子BCL6抑制剂可有效治疗非硬皮病型慢性移植物抗宿主病
2018-10-07 MedSci MedSci原创
中心点:在慢性GVHD小鼠模型中,BCL6的表达对供体骨髓B/T细胞参与生发中心反应必不可少。小分子BCL6抑制剂可调节转录抑制,代表了慢性GVHD的一种新的治疗策略。摘要:类固醇依赖性或难治性cGCHD患者预后不良,仅依鲁替尼获得FDA批准用于该并发症。cGVHD通常是由生发中心(GC)反应所驱动的,在此反应中,滤泡辅助T细胞与GC B细胞相互作用,产生与疾病发病过程相关的抗体。转录共抑制剂BC
在慢性GVHD小鼠模型中,BCL6的表达对供体骨髓B/T细胞参与生发中心反应必不可少。
小分子BCL6抑制剂可调节转录抑制,代表了慢性GVHD的一种新的治疗策略。
摘要:
类固醇依赖性或难治性cGCHD患者预后不良,仅依鲁替尼获得FDA批准用于该并发症。cGVHD通常是由生发中心(GC)反应所驱动的,在此反应中,滤泡辅助T细胞与GC B细胞相互作用,产生与疾病发病过程相关的抗体。
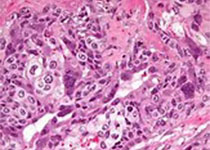
转录共抑制剂BCL6是BTB/POZ转录因子家族的成员,是GC反应中免疫细胞的主要调控因子。研究人员发现BCL6在供体T细胞和B细胞中的表达对cGVHD的发展必不可少,提示BCL6或可作为cGVHD的治疗靶点。
小分子BCL6抑制剂可逆转与强烈的GC反应相关的闭塞性细支气管炎的多器官系统损伤小鼠模型的活跃的cGVHD,但对以硬皮病为主要表现的cGVHD小鼠模型没有明显疗效。
对于由抗体驱动cGVHD的cGVHD患者,靶向BCL6代表一种新的特异性针对GC调控的治疗方法,可拓展至当下可用的二线药物。
Katelyn Paz, et al. Small-molecule BCL6 inhibitor effectively treats mice with non-sclerodermatous chronic graft-versus-host disease. Blood 2018 :blood-2018-03-839993; doi: https://doi.org/10.1182/blood-2018-03-839993
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BCL6抑制剂#
26
#小分子#
33
#BCL6#
33
#抑制剂#
24
#植物#
30
#硬皮病#
32
#宿主#
31
#移植物抗宿主病#
31
#慢性移植物抗宿主病#
42
#有效治疗#
16