中草药改善糖尿病性勃起功能障碍?
2021-11-23 August MedSci原创
糖尿病性勃起功能障碍(DIED)被认为是糖尿病(DM)的常见并发症之一。其发病机制可能与神经、血管、血管内皮、内分泌等因素有关。
糖尿病性勃起功能障碍(DIED)被认为是糖尿病(DM)的常见并发症之一。其发病机制可能与神经、血管、血管内皮、内分泌等因素有关。流行病学调查显示,在当今社会,男性DM患者勃起功能障碍(ED)的发生率已达到35%~90%,是非男性勃起功能障碍(ED)的1.9~4倍。由于DM本身引起的各种复杂的血管和神经病变,死亡比普通ED更难治疗。目前,血管内皮功能障碍和血小板活化异常已被证明是DIED的重要机制,上述机制被认为与中医所说的活血阻络相似。同时活血化瘀中药可在一定程度上改善高血糖时血管内皮功能。但活血化瘀中药对DIED血管内皮功能影响的研究较少。
蛋白激酶C (PKC)信号通路作为重要的细胞内信号转导通路,在细胞凋亡、神经兴奋性、细胞增殖分化、基因表达和细胞坏死等方面发挥着关键作用。活血通络七味汤的主要作用是活血通络、散瘀止风。这种治疗可以有效改善ED患者的症状,对DIED患者有很好的治疗效果。为进一步探讨活血通络七味汤治疗DIED的作用机制,设计了相关的动物实验。链脲佐菌素(STZ)诱导大鼠模型,阿扑吗啡(APO)筛选。活血通络七味汤对勃起状态、血管内皮损伤标志物、内皮细胞超微结构、甘油二酯蛋白及mRNA表达的影响 (DAG)、PKCβ、核转录因子(NF-κB)、细胞间黏附分子-1(ICAM-1) 观察 DIED 大鼠,探讨活血通络七味汤改善 DIED 的机制。
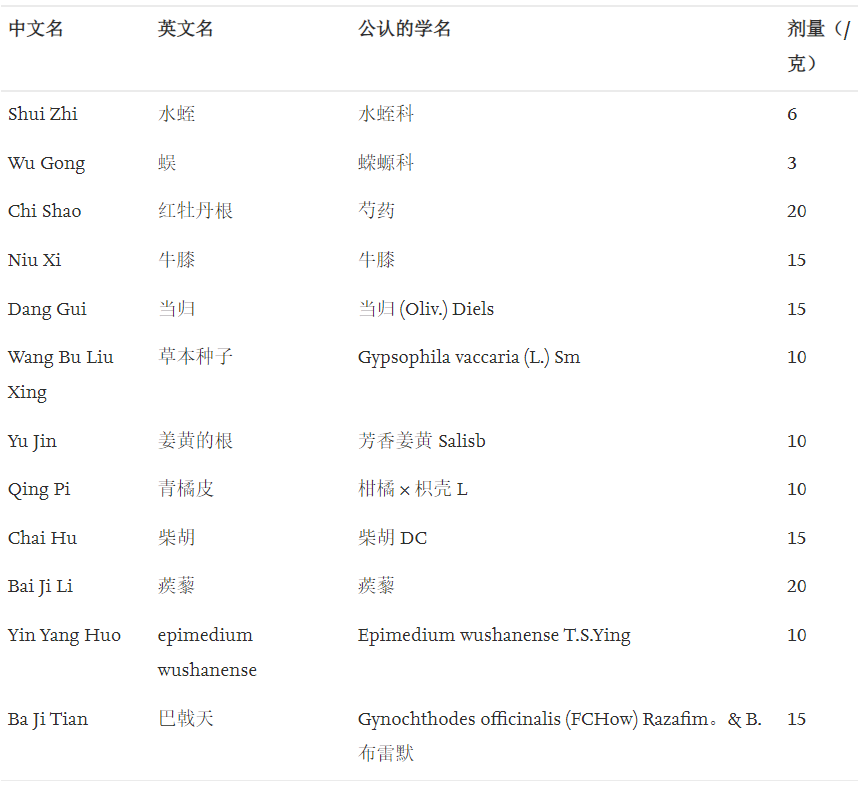
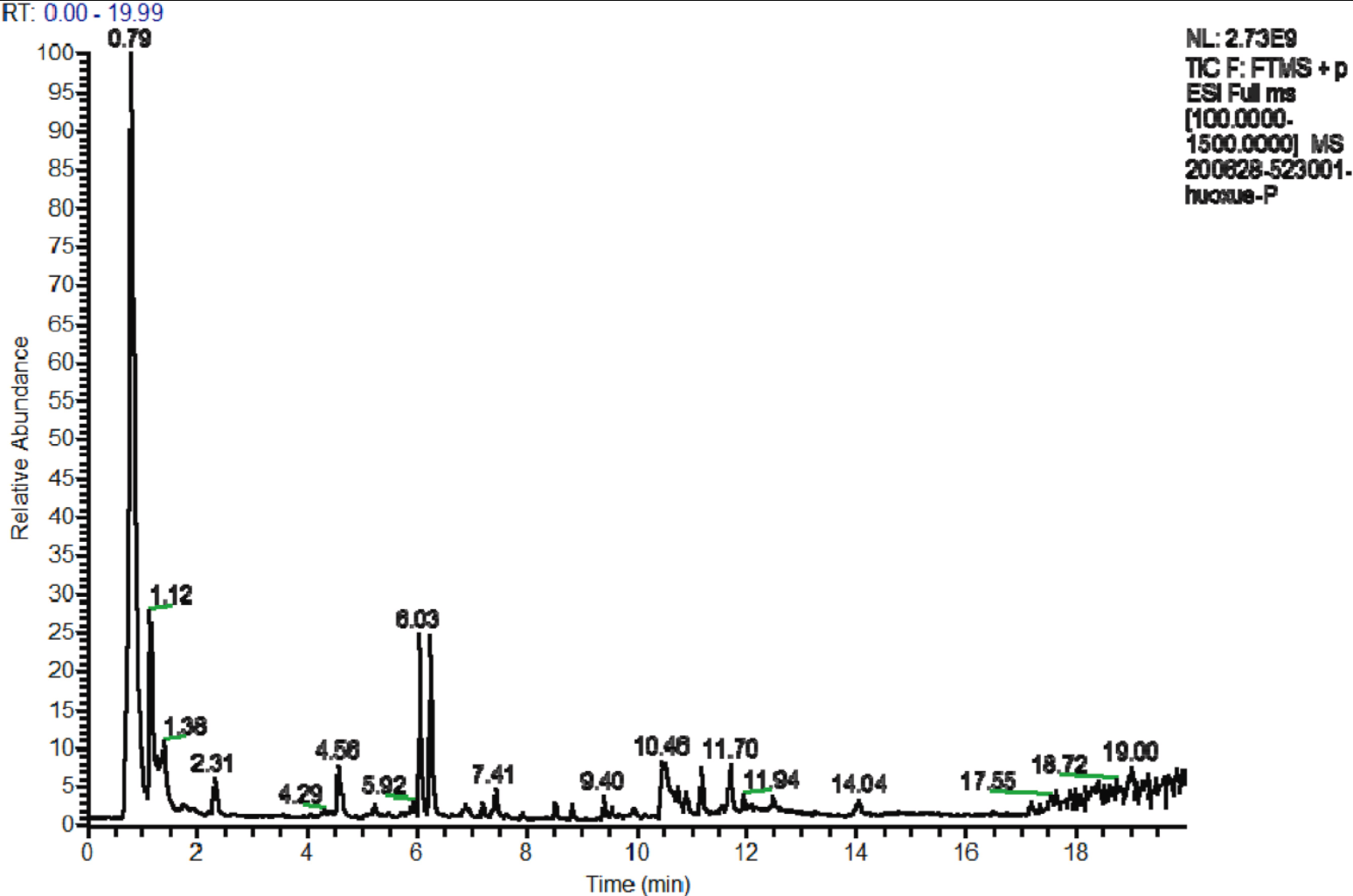
材料和方法:采用高效液相色谱-串联质谱法(HPLC-MS/MS)对活血通络七味汤的化学成分进行了鉴定。链脲佐菌素(STZ)诱导大鼠模型,阿扑吗啡(APO)筛选。通过酶联免疫吸附试验(ELISA)研究血清sE-选择素、赖氨酰氧化酶-1(LOX-1)、丙二醛(MDA)等血管内皮损伤标志物及氧化应激相关指标。通过电子显微镜和HE染色检查海绵体的内皮细胞和超微结构。Western blotting检测蛋白和mRNA的表达 (WB) 和实时定量聚合酶链反应 (RT-qPCR)。

研究结果显示,M组大鼠血清中sE-选择素、LOX-1、细胞间粘附分子-1(sICAM-1)、内皮微粒(EMPs)、P-选择素(CD62P)和MDA水平显着高于K组大鼠,而超氧化物歧化酶(SOD)水平显着下降。此外,PKC通路被激活,相关蛋白和mRNA的表达增加。活血通络七味汤和LY333531干预8周后L、D、G组血清sE-选择素、LOX-1、sICAM-1、EMPs、CD62P、MDA水平显着低于M组,SOD水平显着升高,蛋白激酶C(PKC)通路受到抑制改善大鼠的勃起功能。
基于 HPLC-MS/MS 的活血通络芪味汤正离子色谱分析:
综上所述,发现 DIED 的机制与血管内皮损伤和 PKCβ 信号通路激活引起的异常血小板激活有关。活血通络七味汤可抑制 DIED 大鼠 PKCβ 信号通路相关分子的蛋白和 mRNA 表达,促进血管内皮损伤,增强抗氧化能力,阻止血小板活化,从而改善 DIED 大鼠的勃起功能。
原文:Li X, Feng JL, Chen ZL, Bao BH, Dai HH, Meng FC, Deng S, Wang B, Li HS, Wang JS. Mechanism by which Huoxue Tongluo Qiwei Decoction improves the erectile function of rats with diabetic erectile dysfunction. J Ethnopharmacol. 2022 Jan 30;283:114674. doi: 10.1016/j.jep.2021.114674. Epub 2021 Sep 21. PMID: 34560214.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#草药#
34
#勃起#
38
#功能障碍#
37
#勃起功能#
56
这个有点意思
73