Thorac Cancer:ALK阳性是I期完全切除的肺腺癌患者无复发生存期(RFS)负性预测指标
2022-03-16 网络 网络
研究表明,I期切除肺腺癌患者中,ALK阳性患者无复发生存期(RFS)更差,高级别组织学亚型和从不吸烟跟ALK阳性相关。
间变性淋巴瘤激酶(ALK)在切除后的肺癌中的临床和预后影响尚不清楚。近期,Thoracic Cancer杂志上发表了一项研究成果,主要是评估ALK阳性在完全切除肺腺癌患者中的预后和预测意义。
我们回顾性筛查197例肺腺癌患者,他们接受了完整的手术切除,并测试了他们的ALK状态。探索ALK阳性状态对无复发生存期(RFS)和总生存期(OS)的影响,以及预测因素。

在197例患者中,有36例(18%)ALK阳性。而在仅限于I期患者中,ALK阳性24例(19.4%),ALK阴性100例(80.6%)。
ALK阳性组和ALK阴性组在总患者队列中的OS和RFS率无显著差异(5年OS: ALK阳性组77.4% vs. ALK阴性组80.9%,p = 0.512;5年RFS: ALK阳性患者48.8% vs. ALK阴性患者63.5%,p = 0.123)。这种趋势在病理II-III期患者中相似(5年OS: ALK阳性患者70.7% vs ALK阴性患者67.2%,p = 0.817 5年RFS: ALK阳性患者33.3% vs ALK阴性患者38.8%,p = 0.965)。
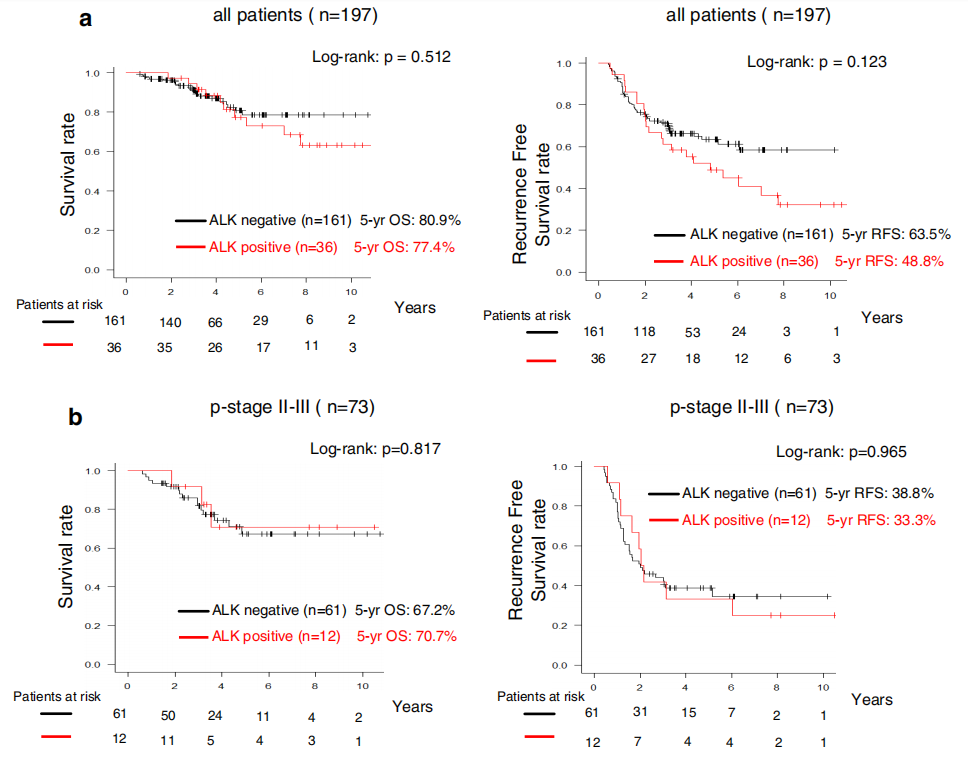
当局限于病理I期患者时,ALK阳性组和ALK阴性组的RFS率有显著差异(5年RFS: ALK阳性组和ALK阴性组的RFS率分别为55.9%和78.8%,p = 0.018)。而OS在ALK阳性组和ALK阴性组之间无显著差异(5年OS: ALK阳性组81.2% vs. ALK阴性组89.8%,p = 0.226)。

多因素分析显示ALK阳性状态(危险比[HR]=3.431, p = 0.009)是RFS的独立预后因素。
高级别组织学亚型(优势比[OR]=5.988, 95% CI: 2.083-14.29, p<0.001)和从不吸烟患者(OR=4.292, 95% CI: 1.280-14.29, p = 0.018)被发现可独立预测ALK阳性状态。

综上,研究表明,I期切除肺腺癌患者中,ALK阳性患者无复发生存期(RFS)更差,高级别组织学亚型和从不吸烟跟ALK阳性相关。
原始出处:
Fujibayashi Y, Tane S, Kitazume M, Kuroda S, Kimura K, Kitamura Y, Nishio W. Resected stage I anaplastic lymphoma kinase-positive lung adenocarcinoma has a negative impact on recurrence-free survival. Thorac Cancer. 2022 Mar 10. doi: 10.1111/1759-7714.14365. Epub ahead of print. PMID: 35274461.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ALK阳性#
54
#THORAC#
57
#生存期#
60
#预测指标#
44