IBD: 血清二肽基肽酶4是一种新的炎症性肠病疾病活动和预后的预测指标
2020-10-25 MedSci原创 MedSci原创
克罗恩病(CD)和溃疡性结肠炎(UC)是一组特发性自身免疫性炎症性肠病(IBDs)的一部分,其特征是疾病发作随后缓解。
克罗恩病(CD)和溃疡性结肠炎(UC)是一组特发性自身免疫性炎症性肠病(IBDs)的一部分,其特征是疾病发作随后缓解。疾病爆发通常涉及粘膜炎症,最终导致肠上皮的结构和功能改变。因此,IBD治疗的主要目标是诱导和维持临床缓解。尽管如此,即使在有效治疗的情况下,亚临床炎症也可能持续存在,导致复发的风险增加以及将治疗升级为免疫调节剂,生物疗法甚至手术的风险也不断提高。内窥镜检查过程中收集的活检样本的检查仍然是评估肠道炎症的金标准,但它具有侵入性,如果内窥镜未能到达病变部位,可能会导致误导性结果。在这种情况下,生物标志物已成为疾病活动,复发风险,治疗需求增加和/或对治疗反应的重要指标。血清二肽基肽酶4(DPP-4)作为炎症性肠病(IBD)的生物标记物引起了研究人员的兴趣,因为该蛋白酶可以使参与炎症级联反应的几种肽的失活。因此,本项研究就此进行了相关探究。

研究人员使用临床指标评估了由195名患者组成的两个前瞻性队列(101名患有克罗恩病[CD],94名患有溃疡性结肠炎[UC]),并随访评估治疗的效果。在基线时有68例患者接受了内镜检查。在第二批46名经过生物学治疗的患者中,评估了治疗反应。在基线和随访期间对血清DPP-4,C反应蛋白(CRP)和粪便钙卫蛋白水平进行了定量分析。
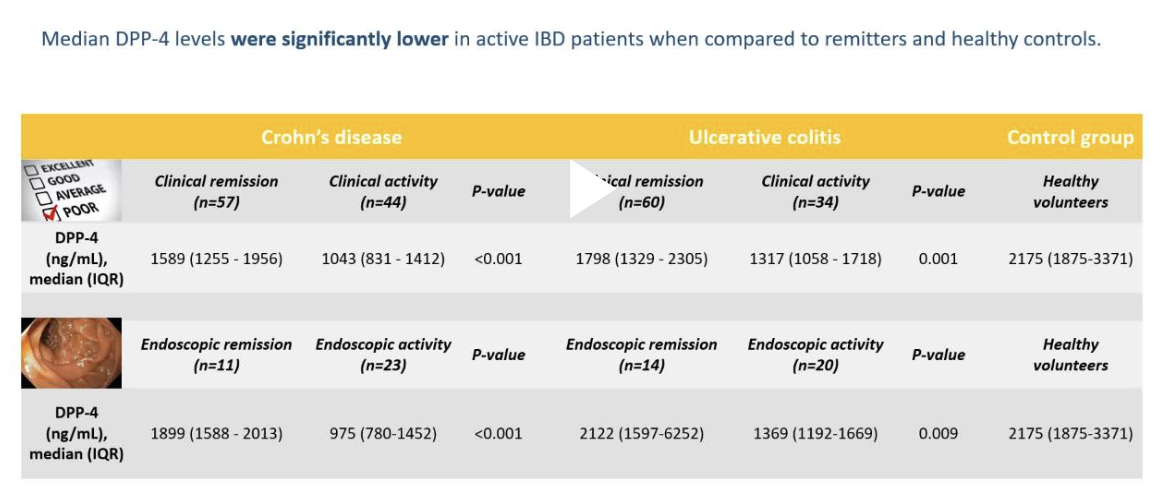
结果显示:与缓解者相比,活跃IBD患者的中位DPP-4水平显着降低(CD:1043 [831–1412] vs 1589 [1255-1956] ng / mL;P <0.001; UC:1317 [1058-1718] vs 1798[1329–2305] ng / mL;P = 0.001)和健康对照组(2175 [1875–3371] ng / mL)。实际上,DPP-4能够区分临床和内窥镜检查活动与缓解之间的关系,曲线下面积(AUC)为0.81 / 0.93(CD)和0.71 / 0.79(UC),此外,对治疗的有反应的患者DPP-4水平更高,而在UC患者中,DPP-4水平更高(1467 [1301–1641] vs 1211 [1011-1448] ng / mL;P <0.001),而CD患者(1385 [1185–1592] vs 1134 [975-1469] ng / mL;P = 0.015)。
血清DPP-4可用作IBD活性和生物治疗反应的非侵入性生物标志物,并且可以作为治疗升级的预测指标,尤其是与其他生物标志物组合使用时。
原始出处:
Pedro Pinto-Lopes. Et al. Serum Dipeptidyl Peptidase 4: A Predictor of Disease Activity and Prognosis in Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疾病活动#
34
#IBD#
37
#预测指标#
47
#炎症性#
35