Neurology:1990-2019年全球缺血性卒中疾病负担:中国年龄标准化发病率(ASIR)增长最为显著,全球范围内女性缺血性卒中负担较大,老龄尤甚
2022-01-17 Naomi MedSci原创
近日,有研究人员对GBD 2019年的数据进行了缺血性卒中的分析, 在中等、中-高等SDI地区,ASIR、ASDR和年龄标化DALY率仍然较高。全球范围内,女性缺血性卒中负担大于男性,50岁以上尤甚。
卒中是成人残疾的主要原因,也是世界范围内死亡的主要原因。根据2019年全球疾病负担(GBD)的调查结果,卒中是1990年-2019年50岁及以上人群残疾调整生命年(DALY)的首要原因之一。
据流行病学研究报告,缺血性卒中占所有卒中病例的85%。因此,缺血性卒中已被联合国视为减轻非传染性疾病负担的优先目标。然而,目前的努力将不足以在2030年前实现可持续发展目标。此外,由于缺血性卒中可有效预防的,世界各地的人口正在老龄化,所有国家都在继续流行病学过渡,因此,每年定期对缺血性卒中进行重新评估,包括最新的风险估计,这对于估计预防进展至关重要。
关于全球缺血性卒中负担的研究主要集中在1990年-2019年期间缺血性卒中负担的总百分比变化,但没有人通过对全球疾病负担(GBD)2019年数据集的数据进行线性回归来计算全球缺血性卒中负担的年度估计百分比变化(EAPC)。EAPC提供的是时间趋势的年度变化,而不是研究期间的总百分比变化,这提供了更准确的信息。此外,以往的文献没有阐明缺血性卒中的年龄标化率与社会发展指数(SDI)之间的Pearson相关系数。研究还将缺血性卒中的估计发病率和死亡率以及因缺血性卒中估计的DALYs与基于SDI预测的发病率和死亡率进行了比较。
自2017年GBD以来,尚无发布缺血性卒中的描述性流行病学和趋势的全面更新,从性别、年龄和社会发展指数(SDI)的角度研究全球、地区和国家层面的缺血性卒中负担。GBD 于2019年评估了全球204个国家和地区的369种人类疾病和伤害的负担。GBD数据每年更新,并适当改变方法。近日,有研究人员基于GBD 2019年的数据,通过确定缺血性卒中的时间趋势来评估缺血性卒中的负担在性别、年龄和SDI方面,全球、区域和国家层面的缺血性卒中的发病率和死亡率以及伤残调整寿命年(DALY)。
数据是从GBD 2019年数据集中提取的。计算估计的年度百分比变化(EAPC)以评估缺血性卒中的发病率、死亡率和残疾调整寿命年(DALY)趋势。测量方法按性别、地区、国家、年龄和SDI分层。
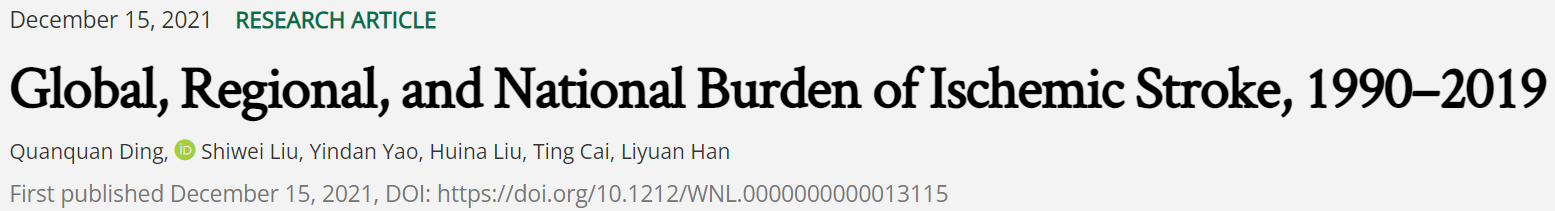
- 从1990年到2019年,缺血性卒中的全球年龄标准化发病率(ASIR)下降,EAPC为-0.43[95%可信区间(CI),-0.54到-0.32]。
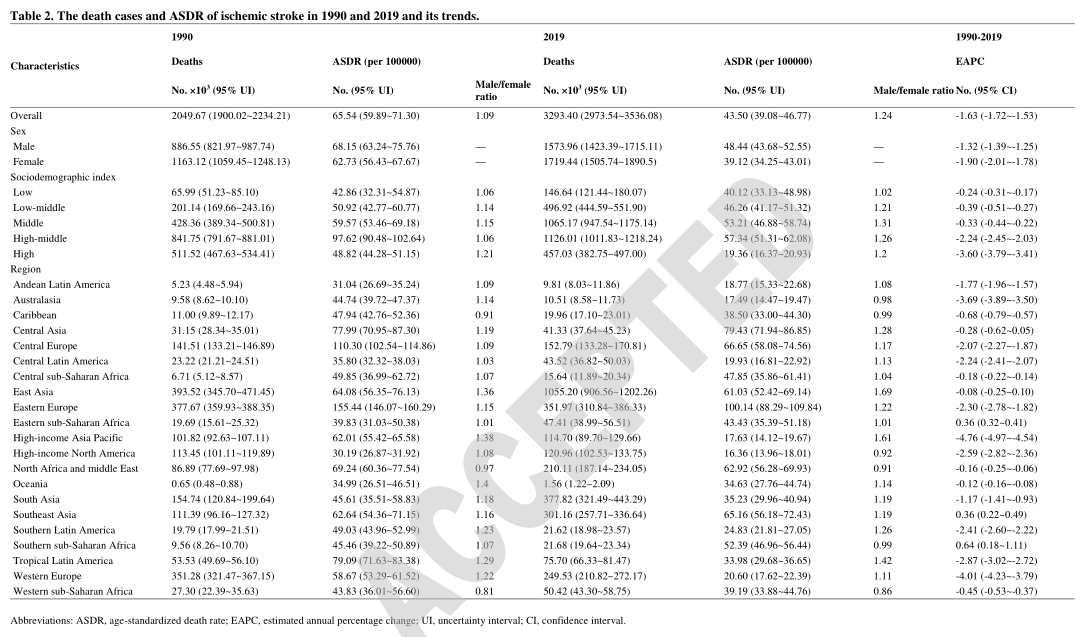
- 高-中等、中等社会发展指数(SDI)地区的缺血性卒中ASIR、ASDR和年龄标化DALY率明显高于其他SDI区域。从地区来看,2019年东亚缺血性卒中的ASIR最高,1990-2019年ASIR的增幅最大。
- 在全国范围内,埃及(EAPC,1.40;95%CI,1.27至1.52)和中国(EAPC,1.10;95%CI,1.00至1.20)缺血性卒中的ASIR增加最为显著。
- 在全球范围内,缺血性卒中的发病率随着年龄的增长而增加,特别是在50-69岁或以上的女性中。
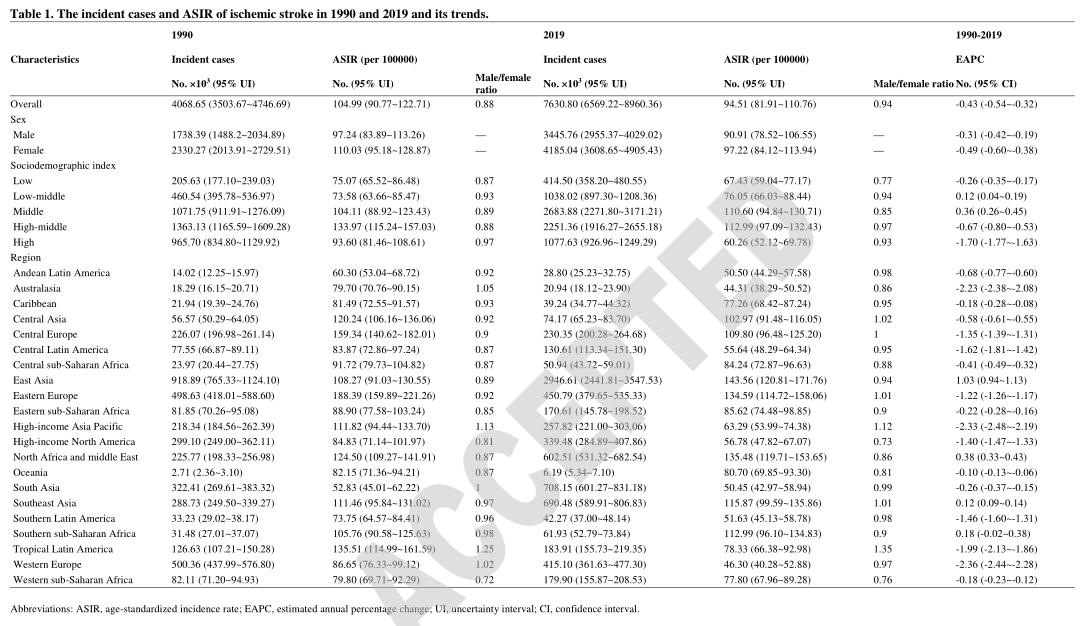
- 1990年至2019年,全球年龄标准化死亡率(ASDR)下降,EAPC为-1.63(95%CI,-1.72至-1.53)。
- 在撒哈拉以南非洲南部、撒哈拉以南非洲东部和东南亚,ASDR和年龄标准化的DALY比率增加最多。
在中等、中-高等SDI地区,ASIR、ASDR和年龄标化DALY率仍然较高。东亚、撒哈拉以南非洲南部、撒哈拉以南非洲东部和东南亚的缺血性卒中负担最大。在全球范围内,女性缺血性卒中的负担比男性更大,特别是那些50-69岁或更年长的人。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#缺血性#
45
#Neurol#
49
#标准化#
51
#发病率#
51
#缺血性卒#
47
#疾病负担#
38
涨知识了
90
学习了 谢谢分享
64
学习了,谢谢分享
84
学习了
92