BMJ:肾衰竭患者接受移植或继续透析的预后差异
2022-03-07 MedSci原创 MedSci原创
对于大多数肾衰竭患者,肾移植仍然是降低全因死亡率的最佳治疗方式,但某些亚组患者生存期改善不显著。鉴于供体器官短缺,需要进一步考察影响肾衰患者移植后生存期的影响因素。

器官移植是肾衰竭患者的首选治疗选择,可改善大多数适合移植患者的死亡率和生活质量,但并非所有肾衰竭患者都有机会接受肾移植手术。截至2019年12月31日数据显示,英国有28303 名肾衰竭患者接受血液透析或腹膜透析,截至2021年3月31日,只有3525名患者正在积极等待肾移植手术,并且移植后患者需克服全身麻醉、肾移植手术和/或长期免疫抑制相关的并发症。近日研究人员比较了接受移植与继续透析对肾衰竭患者生存的影响。

本次研究为系统回顾和荟萃分析,收集MEDLINE、Ovid Embase、科学网、Cochrane相关研究。比较符合肾移植条件的肾衰竭患者移植或继续透析后的全原因死亡率差异。
总计48项非随机对照试验纳入本次研究,包含1245850 名患者。总的来说,与透析相比,92%(n=44/48)的研究发现移植与相关的长期(至少一年)生存相关,但其中有11项确定与继续透析相比,移植在改善患者生存方面无统计学意义。对18项研究进行荟萃分析显示,肾移植可提高生存率(死亡风险比0.45),在亚组/敏感性分析或元回归分析后仍存在显著的异质性。
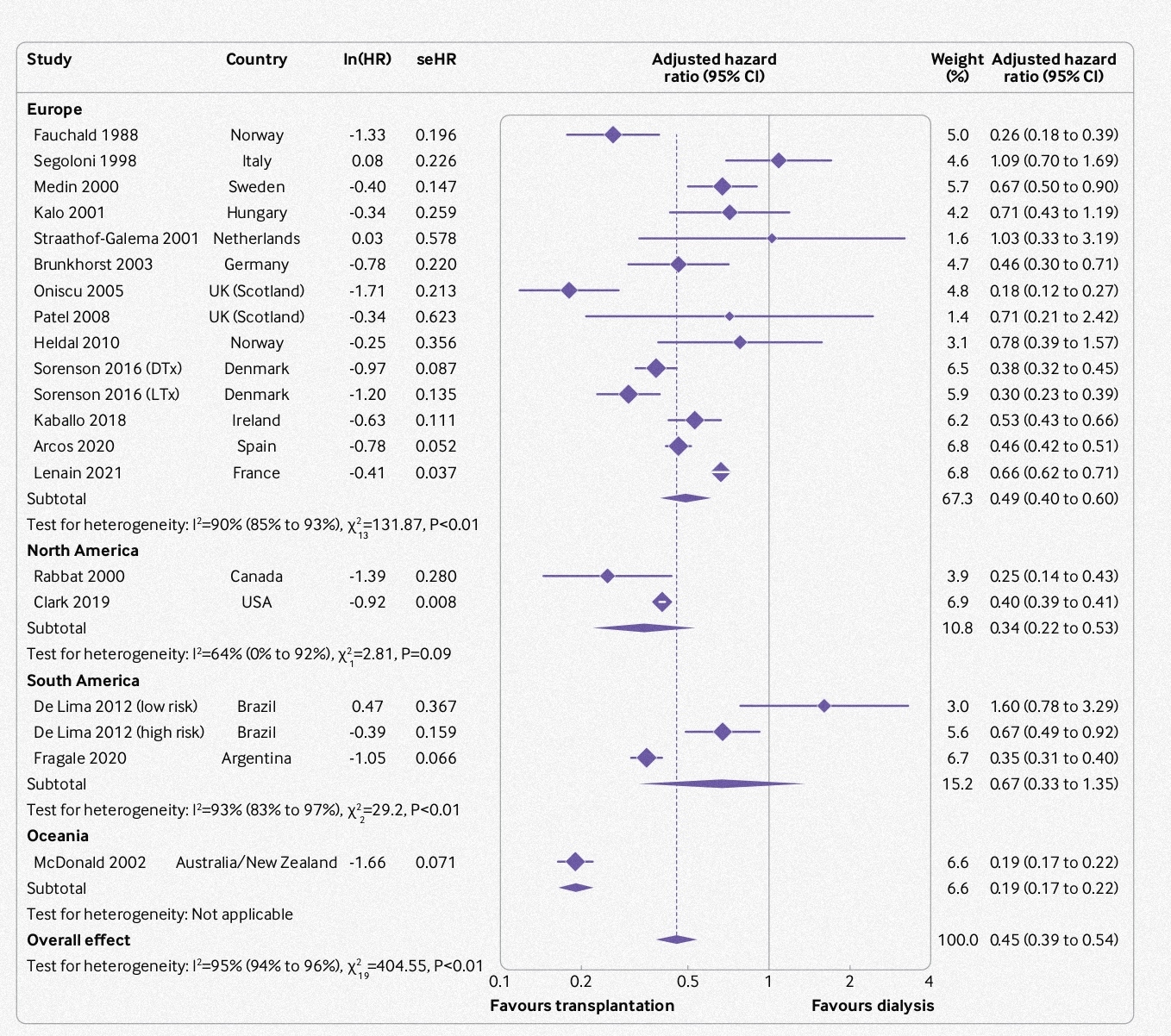
不同地域患者移植后生存期差异
研究发现,对于大多数肾衰竭患者,肾移植仍然是降低全因死亡率的最佳治疗方式,但某些亚组患者生存期改善不显著。鉴于供体器官短缺,需要进一步考察影响肾衰患者移植后生存期的影响因素。
原始出处:
Daoud Chaudhry et al. Survival for waitlisted kidney failure patients receiving transplantation versus remaining on waiting list: systematic review and meta-analysis. BMJ,01 March 2022。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMJ#
53
#预后差异#
57
学习了
46
#肾衰竭#
0
码住
66
有用知识
45
学习了
53
#学习#
53