CGH: 非酒精性脂肪肝与严重 COVID-19 之间没有因果关系
2022-06-19 xuyihan MedSci原创
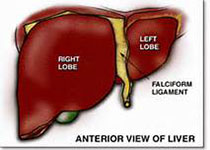
NAFLD一般指非酒精性脂肪性肝病。 非酒精性脂肪性肝病(NAFLD)是指除外酒精和其他明确的损肝因素所致的肝细胞内脂肪过度沉积为主要特征的临床病理综合征。
由SARS-CoV-2病毒感染引起的2019 年冠状病毒病 (COVID-19) 对全球健康构成严重威胁。了解严重COVID-19与患者健康状况之间的关系是 COVID-19 治疗和管理的关键。识别风险因素,尤其是那些可以改变的因素,有助于制定疾病预防策略。迄今为止的大量研究表明,严重的 COVID-19 与年龄较大,男性、肥胖和高血压有关。据估计,全世界大约25%的人口患有NAFLD,NAFLD 是否是严重 COVID-19 疾病的危险因素一直存在长期争论。许多观察性研究表明,NAFLD 患者患严重 COVID-19 的风险显着增加。但是非酒精性脂肪性肝病 (NAFLD) 是否会增加严重 COVID-19 的风险仍不清楚。

为了完成本项研究,研究人员进行了大规模的样本孟德尔随机化分析(TSMR),以检查 NAFLD、血清丙氨酸氨基转移酶、脂肪变性等级、NAFLD 活动评分或纤维化阶段与严重COVID-19之间是否存在因果关系。为了最大限度地发挥这种分析的能力,研究人员进行了全基因组荟萃分析,以确定与 NAFLD 相关的单核苷酸多态性。同时研究人员还研究了 NAFLD 的 20 种主要合并症因素对严重 COVID-19 的影响。

单变量分析表明 NAFLD 与重症 COVID-19 之间存在显着关联(优势比 [OR],3.06;P= 1.07×10–6)。然而,在调整人口统计学和合并症因素后,这种关联消失了(OR,1.57;P=.09)。TSMR研究表明 NAFLD (OR, 0.97; P= .61)、丙氨酸氨基转移酶水平 (OR, 1.03; P= .47)、脂肪变性等级 (OR, 1.08; P= .41)、NAFLD 活动评分 (OR, 1.02;P= .39)和纤维化阶段(OR,1.01;P= .87)与严重的 COVID-19无关。在所有与 NAFLD 相关的合并症因素中,体重指数(OR,1.73;P =7.65 × 10 –9 )、腰围 (OR, 1.76; P = 2.58 × 10 –5 ) 和臀围 (OR, 1.33; P = 7.26 × 10 –3 ) 是唯一显示对严重 COVID-19有因果影响的因素。

本项研究表明没有证据支持NAFLD是COVID-19的因果风险因素。先前观察到 NAFLD 与 COVID-19 之间的关联可能归因于 NAFLD 与肥胖之间的相关性。
原始出处:
Jiuling Li. Et al. Mendelian Randomization Analysis Reveals No Causal Relationship Between Nonalcoholic Fatty Liver Disease and Severe COVID-19. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#酒精性#
48
#非酒精性#
44
#CGH#
50
#酒精性脂肪肝#
39
好文章,谢谢分享。
55