Cell Host Microbe:清华大学医学院程功研究组发现一种肠道菌可调控蚊虫传播病毒
2019-01-09 佚名 病毒学界
蚊子是多种烈性病毒的主要携带者和传播者,蚊子的肠道可有效抵御病毒感染,是病毒感染蚊虫的最主要生理屏障。了解肠道共生菌、媒介蚊虫和病毒之间的互作关系对于理解病毒的致病机制以及疫情的防控具有重要意义。
蚊子是多种烈性病毒的主要携带者和传播者,蚊子的肠道可有效抵御病毒感染,是病毒感染蚊虫的最主要生理屏障。了解肠道共生菌、媒介蚊虫和病毒之间的互作关系对于理解病毒的致病机制以及疫情的防控具有重要意义。2018年12月27日,清华大学医学院程功课题组在微生物领域顶级期刊《Cell Host & Microbe》在线发表了题为A Gut Commensal Bacterium Promotes MosquitoPermissiveness to Arboviruses的研究论文,该论文将在2019年1月份正式见刊发表。研究首次鉴定出一种蚊虫肠道共生菌粘质沙雷氏菌(Serratia marcescens)可通过分泌增效因子蛋白SmEnhancin决定蚊虫对病毒的易感性,最终调控蚊虫传播病毒的能力,为蚊媒病毒的防控提供了新的科学依据。
研究背景
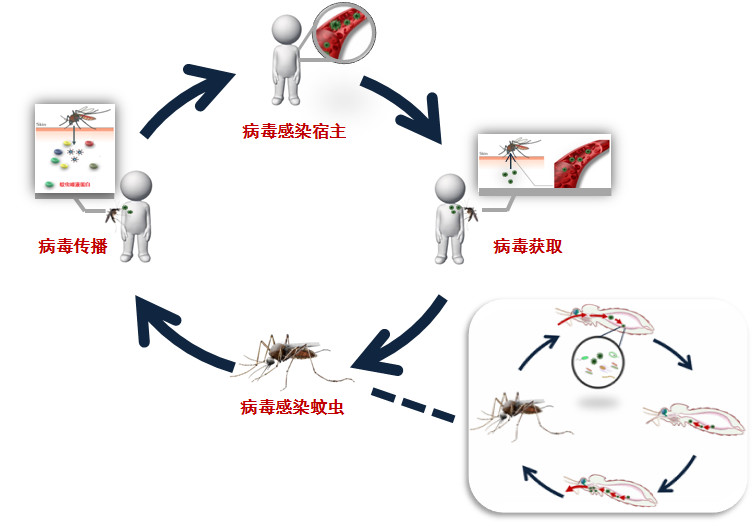
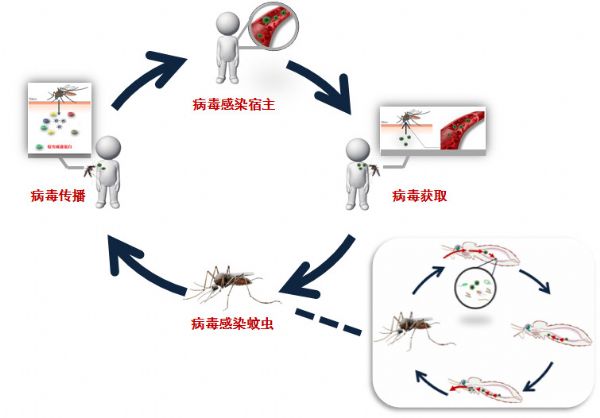
在自然界中,蚊子是多种烈性病毒的主要携带者和传播者。这些蚊媒病毒感染人体后可以引起多种烈性的临床症状,诸如脑炎、脑膜炎、出血热等,重度感染可以导致非常高的死亡率。蚊媒病毒在宿主和蚊虫之间传播循环(图1)。在这个过程中,蚊子可以通过叮咬吸血从病人的血液中获取病毒,病毒进入到蚊子体内,感染蚊子中肠的上皮细胞,继而扩散并感染蚊子的唾液腺,使蚊子具备携带及传播病毒的能力。因此,蚊子的肠道组织是病毒首先接触并感染的器官。实际上,蚊子的肠道可有效抵御病毒感染,是病毒感染蚊虫的最主要生理屏障,蚊虫的肠道屏障可有效决定蚊虫对病毒的易感性。
图1. 蚊媒病毒传播循环
蚊虫肠道中存在种类丰富、数目众多的肠道微生物菌群。之前,清华大学程功实验室已经鉴定出多种维持蚊虫肠道微生物菌群稳态的分子机制,包括:鉴定出多种C型凝集素是维持蚊虫肠道微生物菌群稳态的关键分子(Pang et al., 2016,Nature Microbiology, 1: 16023);发现蚊虫肠道通过活性氧ROS系统调节肠道微生物稳态的分子机制 (Xiao et al., 2017,Nature Microbiology, 2: 17020),以上研究为理解“蚊虫-肠道微生物-病毒”的互作关系奠定了坚实的基础。
研究结果
在这项研究中,研究人员首先使用抗生素去除埃及伊蚊洛克菲勒株的肠道微生物菌群,发现抗生素处理可以明显降低登革病毒感染蚊虫,并据此推测该伊蚊肠道中存在能辅助病毒感染蚊虫的肠道共生菌。研究人员分别评估了21株可培养肠道菌对伊蚊获取蚊媒病毒的影响,发现粘质沙雷氏菌可以显着地增强埃及伊蚊对蚊媒病毒的易感性。这项研究还检测了不同登革发病地区野外来源的伊蚊肠道中粘质沙雷氏菌,发现肠道中该菌含量与登革病毒流行程度存在一定关联。给登革低发地区的野外来源伊蚊饲喂粘质沙雷氏菌,可以增强该伊蚊对登革病毒的易感性。
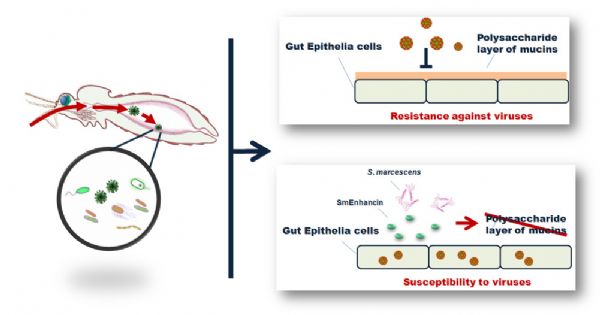
为研究粘质沙雷氏菌辅助登革病毒感染伊蚊的作用机制,研究人员分别研究了粘质沙雷氏菌的菌体固有组分、胞外分泌小分子及蛋白质在辅助病毒感染中的作用,最后发现效应分子在粘质沙雷氏菌的胞外分泌蛋白中。通过进一步分离实验、质谱鉴定以及功能研究,研究人员发现一种细菌分泌蛋白为辅助蚊媒病毒感染作用的关键蛋白,并将其命名为SmEnhancin。进一步研究结果发现,SmEnhancin通过降解蚊虫肠道细胞表面的粘蛋白(Mucin)层从而提高肠道细胞对病毒的易感性。这项研究首次发现了肠道细菌编码的蛋白因子在辅助蚊媒病毒感染中的作用(图2)。
图2. 肠道共生菌粘质沙雷氏菌可通过分泌一种细菌因子SmEnhancin辅助蚊媒病毒感染蚊虫
研究意义&结语
该研究揭示了肠道共生菌、媒介蚊虫和病毒之间的互作关系,阐明了粘质沙雷氏菌通过分泌增效因子影响媒介易感性的分子机制,发现粘质沙雷氏菌与登革热流行存在一定关联。该研究为蚊媒病毒的防控提供了新的科学依据。
清华大学医学院博士后吴葩为本研究第一作者,程功研究员为论文的通讯作者。中国疾控中心刘起勇教授、军事医学科学院赵彤言教授、南方医科大学陈晓光教授、云南省寄生虫病防治所周红宁教授、美国康涅狄格大学医学院王朋华教授为该论文共同作者。
该研究得到国家自然科学基金委重点项目、杰出青年科学基金、科技部重点研发计划、深圳市三名工程、清华大学-北京大学生命科学联合中心的基金资助。
通讯作者简介:
程功研究员于2012年1月起任清华大学医学院研究员、博士生导师。主要致力于蚊媒病毒感染机制与抗病毒免疫研究,从分子层面阐明多种重要蚊媒病毒感染传播的分子机制及宿主免疫保护机制,为重要蚊媒病毒的防治提供生物学基础。程功研究员以通讯作者 (含共同) 或第一作者在Nature、Cell等国际著名期刊发表论文及特邀综述,首次发现寨卡病毒暴发机制、提出针对蚊媒病毒传染病的新型传播阻断策略。
原始出处:Wu P1, Sun P1, Nie K1, et al. A Gut Commensal Bacterium Promotes Mosquito Permissiveness to Arboviruses. Cell Host Microbe. 2018 Nov 28.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
26
#CRO#
26
#Cell#
40
#Micro#
40
#医学院#
35
#肠道菌#
0
#清华#
27