JAHA:莱顿V因子并不改变急性冠状动脉综合征的表型或心肌坏死程度
2021-05-17 MedSci原创 MedSci原创
在伴有急性冠脉综合征的一般人群中,FVL不能区分STEMI或非ST段抬高急性冠脉综合征患者,并且与STEMI患者的心脏坏死标志物峰值无关。
与非ST段抬高的急性冠脉综合征相比,血栓前缺陷莱顿V因子 (FVL)可能导致ST段抬高型心肌梗死(STEMI)风险增高,并可能与更高的血栓负担导致更多的心肌坏死相关。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员从2项急性冠脉综合征患者的临床试验中选取了无心血管病史的患者。FVL被定义为V因子(V R506Q)基因1691核苷酸的G-A的置换。

在总体人群和亚组中,调整了性别、年龄(≥70岁 vs. 70岁)以及在传统心血管危险因素,研究人员计算了比值比,以评估FVL与STEMI之间的相关性,并对比了FVL携带者和非携带者STEMI后的峰值生物标志物水平(即肌酸激酶心肌带和高敏感性肌钙蛋白I或T)。由于肌钙蛋白测定方法的差异,峰值高敏感性肌钙蛋白水平被转换为一个比例尺度。
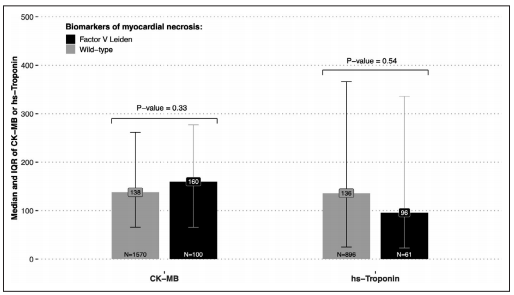
在STEMI患者(6.0%)和非ST段抬高急性冠脉综合征患者(5.8%)中,FVL突变的患病率类似。调整性别和年龄后,FVL与STEMI之间相关性的比值比为1.06(95%CI为0.86-1.30;P=0.59)。亚组分析没有发现任何差异。在STEMI患者中,野生型和FVL携带者肌酸激酶‐心肌带的中位峰值和高敏感性肌钙蛋白比值均无差异(肌酸激酶‐心肌带对应P=0.33;高敏感性肌钙蛋白比值P=0.54)。
由此可见,在伴有急性冠脉综合征的一般人群中,FVL不能区分STEMI或非ST段抬高急性冠脉综合征患者,并且与STEMI患者的心脏坏死标志物峰值无关。
原始出处:
Bakhtawar K. Mahmoodi.et al.Factor V Leiden Does Not Modify the Phenotype of Acute Coronary Syndrome or the Extent of Myocardial Necrosis.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.020025
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#冠状动脉综合征#
31
#AHA#
33
#坏死#
34
#综合征#
24
#表型#
24
已读,真是受益匪浅呀。
50