Circulation:ICD植入同时进行消融可改善合并单形性室速的心肌病患者的综合预后
2022-06-28 MedSci原创 MedSci原创
对于各种病因的心肌病患者,ICD 植入时进行早期导管消融可显著降低 VT 复发、心血管住院及死亡的复合结局。
导管消融作为植入式心律转复除颤器 (ICD) 植入时室性心动过速 (VT) 的一线治疗尚未被纳入临床指南。此外,目前仍缺乏评估 VT 消融在非缺血性心肌病患者中的作用的前瞻性研究。非缺血性心肌病的发病率越来越高,在全球范围内都被推荐接受先进的治疗。
该研究是一项国际性、多中心、随机对照的临床试验,招募了180位有 ICD 植入指征的心肌病和单形性 VT 患者,以评估早期一线消融治疗的作用。共121位患者被随机(1:1)分至消融+ICD 组或常规治疗+ICD 组。拒绝行 ICD 治疗的47位患者在单纯消融治疗后进行前瞻性的随访。主要终点是 VT 复发、心血管因素住院或死亡的复合结局。
随机分组患者的平均年龄是55岁(四分位距 46-64),平均左心室射血分数是40%(四分位距 30%-49%);81%的是男性。35%的患者是缺血性心肌病,30%的患者是非缺血性心肌病,还有35%的患者是致心律失常性心肌病。在植入 ICD 前中位 2 天进行了消融(四分位距 前5天-后14天)。
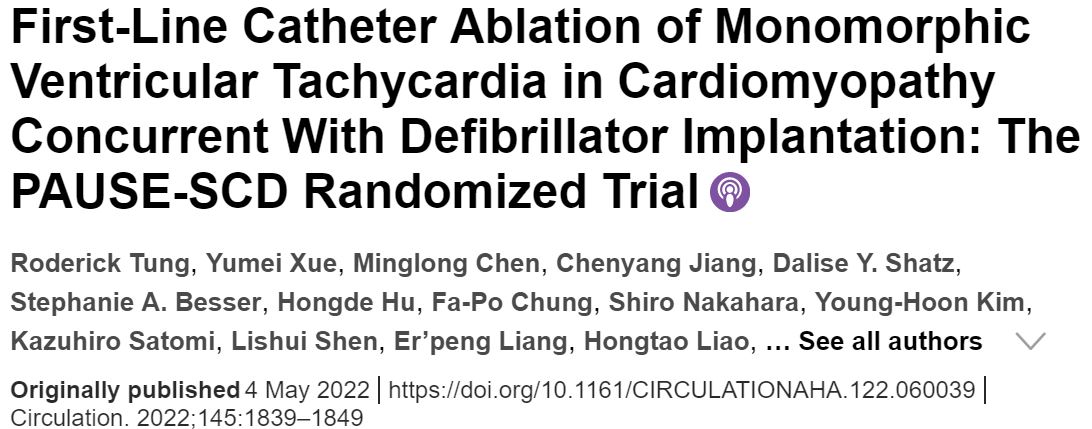
两组患者无复合终点事件生存率
第31天时,消融组和对照组的主要终点发生率分别是49.3%和65.5%(风险比[HR] 0.58,p=0.04)。两组之间的差异主要是消融组的 VT 复发明显减少(HR 0.51,p=0.02)。与对照组相比,在接受消融治疗的患者中观察到 ICD 电击(10.0% vs 24.6%;p=0.03)和抗心动过速起搏(16.2% vs 32.8%;p=0.04)次数均显著降低。
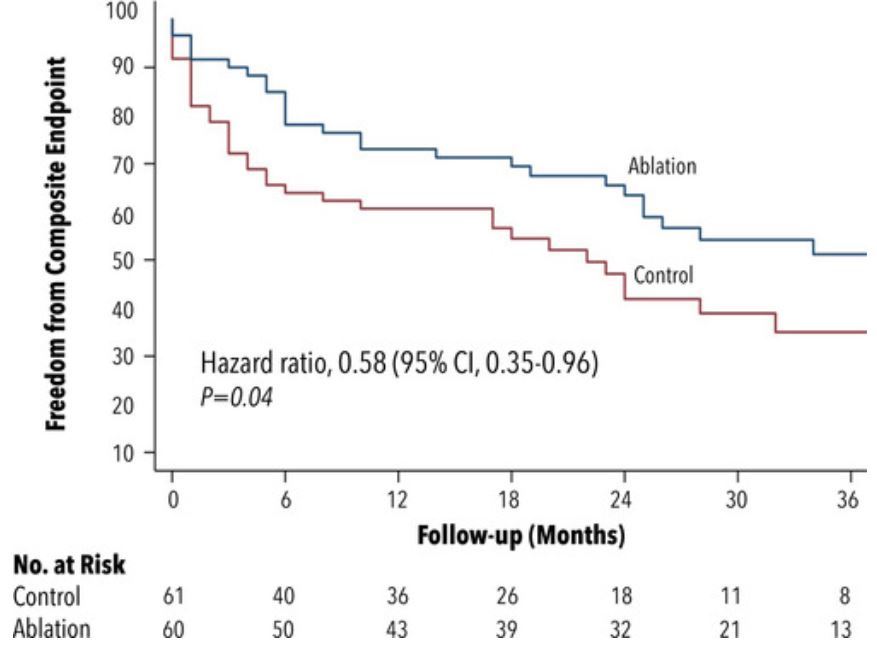
两组无各终点事件的生存率
此外,两组患者的心血管因素住院率(32.0% vs 33.7%,p=0.55)或死亡率(8.9% vs 8.8%,p=0.62)均未观察到显著差异。8.3%的患者发生了消融相关并发症。
总而言之,对于各种病因的心肌病患者,ICD 植入时进行早期导管消融可显著降低 VT 复发、心血管住院及死亡的复合结局。
原始出处:
Roderick Tung, et al. First-Line Catheter Ablation of Monomorphic Ventricular Tachycardia in Cardiomyopathy Concurrent With Defibrillator Implantation: The PAUSE-SCD Randomized Trial. Circulation. 2022;145:1839–1849. https://doi.org/10.1161/CIRCULATIONAHA.122.060039.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ICD#
49
#消融#
50
#室速#
50
#植入#
57
#肌病#
53