European Radiology:Gd-EOB-DTPA增强MRI放射组学对HCC组织学及患者预后的预测
2021-11-03 shaosai MedSci原创
肝细胞肝癌(HCC)是最常见的肝脏恶性肿瘤之一,是全球癌症相关死亡的第三大原因。目前,手术切除和肝移植是HCC患者的有效治疗方式,但术后复发和转移十分常见。
 肝细胞肝癌(HCC)是最常见的肝脏恶性肿瘤之一,是全球癌症相关死亡的第三大原因。目前,手术切除和肝移植是HCC患者的有效治疗方式,但术后复发和转移十分常见。接受肝脏切除术患者术后5年复发率约为70%,肝脏移植术的复发率为25-35%。
肝细胞肝癌(HCC)是最常见的肝脏恶性肿瘤之一,是全球癌症相关死亡的第三大原因。目前,手术切除和肝移植是HCC患者的有效治疗方式,但术后复发和转移十分常见。接受肝脏切除术患者术后5年复发率约为70%,肝脏移植术的复发率为25-35%。
然而,HCC的血管生成与它的发生、发展和转移密切相关。HCC的病理性血管生成过程被称为毛细血管化。在高达90%的晚期HCC中可观察到弥漫性毛细血管化的形成。最近,有专家报道了一种独特的HCC血管化模式,其特点是在病理成像中存在CD34+肿瘤包绕型血管(VETC)。VETC模式影响患者的预后,与HCC转移和复发的增加有显著相关。然而,目前VETC只能通过手术切除后的组织病理学评估来诊断,术前无创预测HCC的VETC具有重要的临床意义。
Gd-EOB-DTPA是一种新型肝胆特异性MRI对比剂,可以提供肝胆病变的功能和结构信息。一些研究报道,Gd-EOB-DTPA增强的MRI可以反映HCC的部分生物学特征,包括组织学等级和微血管侵袭(MVI)。放射组学在HCC中的应用包括鉴别诊断、评估治愈效果和预测早期复发。据我们所知,尚未由研究使用Gd-EOB-DTPA增强MRI放射组学特征预测HCC的VETC和患者预后。
近日,发表在European Radiology杂志的一项研究根据从Gd-EOB-DTPA增强MRI中提取的瘤内和瘤周特征,开发并验证了一个放射组学模型,并评估了该模型术前预测HCC患者的VETC和预后的效能,为HCC患者个性化治疗方案的制定提供了参考依据。
本研究纳入了182名(训练队列:128;验证队列:54)接受术前Gd-EOB-DTPA增强MRI扫描的HCC患者。在肝胆期图像中手动划定感兴趣的体积,包括瘤内和瘤周区域,并从中提取1316个放射组学特征。使用最小绝对收缩和选择算子(LASSO)和多变量逻辑回归来选择有用的特征。使用机器学习算法建立了临床、瘤内、瘤周、联合放射组学和临床放射组学模型。采用Kaplan-Meier生存分析来评估VETC+和VETC-患者的早期复发和无进展生存(PFS)。
在验证队列中,放射组学模型的曲线下面积(AUC)高于使用随机森林的临床模型(所有P < 0.05)。瘤周放射组学模型(AUC = 0.972;95%置信区间[CI]:0.887-0.998)的AUC明显高于瘤内模型(AUC = 0.919; 95% CI: 0.811-0.976)(p = 0.044)。在瘤内或瘤周放射学模型(PR)和联合放射学模型之间的AUC没有明显的差异(p>0.05)。早期复发和PFS在PR预测的VETC+和VETC- HCC患者之间有明显差异(P < 0.05)。PR预测的VETC是早期复发(危险比[HR]:2.08[1.31-3.28];p = 0.002)和PFS(HR:1.95[1.20-3.17];p = 0.007)的独立预测因素。

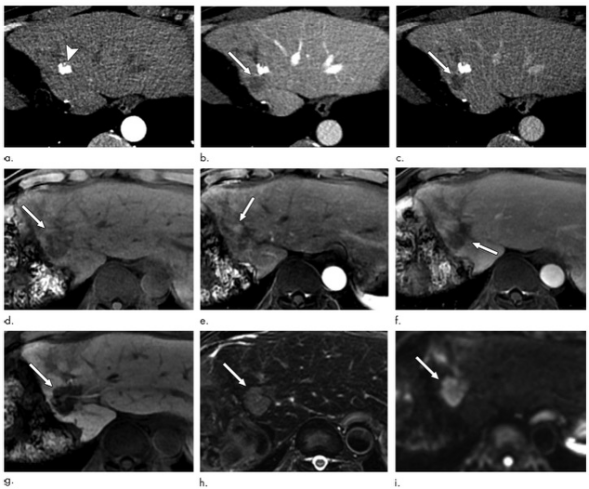
图 a 64岁男性,肝脏右叶、经组织学证实的VETC+HCC。b 一位52岁的女性,肝脏右叶、经组织学证实的VETC-HCC,在肝胆期中也是低信号(白色箭头)。VETC+HCC显示肿瘤细胞群被CD34阳性内皮细胞的完整边缘所包围。VETC-HCC没有形成蜘蛛网状的血管,其内皮细胞为CD34阳性。
本研究表明,瘤内或瘤周放射组学模型在术前预测HCC的VETC和患者预后方面显示出良好的性能。与瘤内模型相比,瘤周放射组学模型的预测能力更佳。因此,本研究提示该模型有助于术前VETC的预测,并可协助临床医生进行治疗方案的制定。
原文出处:
Yixing Yu,Yanfen Fan,Ximing Wang,et al.Gd-EOB-DTPA-enhanced MRI radiomics to predict vessels encapsulating tumor clusters (VETC) and patient prognosis in hepatocellular carcinoma.DOI:10.1007/s00330-021-08250-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#患者预后#
31
#PE#
28
#tPA#
31
#组织学#
33
#HCC#
24