Clin Gastroenterology H:克罗恩病诊断12个月内粪钙卫蛋白水平正常化与疾病进展风险降低有关
2021-09-14 MedSci原创 MedSci原创
目前,全世界每352 人中就有 1 人患有克罗恩病 (CD),CD是一类以复发和缓解反复交替的透壁肠道炎症。
目前,全世界每352 人中就有 1 人患有克罗恩病 (CD),CD是一类以复发和缓解反复交替的透壁肠道炎症。研究表明,大约 60% 的人会出现肠道狭窄或随着时间的推移出现穿透性并发症。此外,10 年后手术风险大约 在50%左右。因此,确定疾病进展的危险因素疾病以及尽早在病程中识别和实施有效的治疗策略具有重要的临床意义。
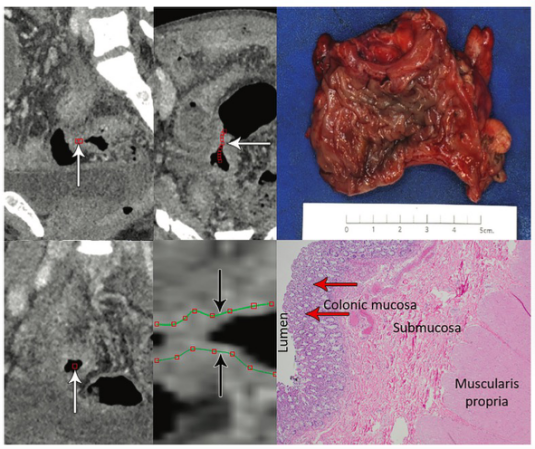
CD的治疗目标是粘膜愈合(MH),但是MH 的评估需要回肠结肠镜检查,这是侵入性且昂贵的检查项目,临床上实施难度较大。因此,粪便钙卫蛋白 (FC) 正成为临床医生治疗CD和监测策略中越来越重要生物指标。粪便中 FC 的水平与与 CD 中粘膜炎症的存在和程度有关。因此,本项研究旨在探究CD 诊断后 12 个月内 FC 的正常化是否与疾病进展的减少有关。
研究人员在英国的三级 IBD 中心进行了一项回顾性队列研究,将2005 年至 2017 年诊断出的所有 CD 事件的患者纳入本项研究。诊断时 FC 测量值≥250 μg/g 且在诊断后的前 12 个月内至少进行了 1 次 FC 测量和 > 12 个月的随访的患者被认为是符合标准的患者。然后研究人员使用患者诊断后 12 个月内的最后一次 FC来判断患者是否达到FC正常化(临界值 <250 μg/g)。主要观察终点是首次疾病进展的时间(蒙特利尔病行为 B1 进展到 B2/3、B2 到 B3,或出现新的肛周疾病;以及出现CD 相关手术;或 CD 相关住院)的时间。

最后本项研究共纳入375 例患者,中位随访时间为 5.3 年。43.5% 的患者在诊断后 12 个月内 FC 正常化。FC 水平正常的患者疾病进展的风险显着降低(风险比 [HR],0.36;95% CI,0.24-0.53;P < .001)。他们出现任何一个观察终点的进展风险也较低(蒙特利尔行为进展或新的肛周疾病 HR,0.22;95% CI,0.11–0.45; P < .001;住院 HR,0.33;95% CI,0.21 –0.53;P <.001;手术 HR,0.39;95% CI,0.19–0.78;P = .008 )
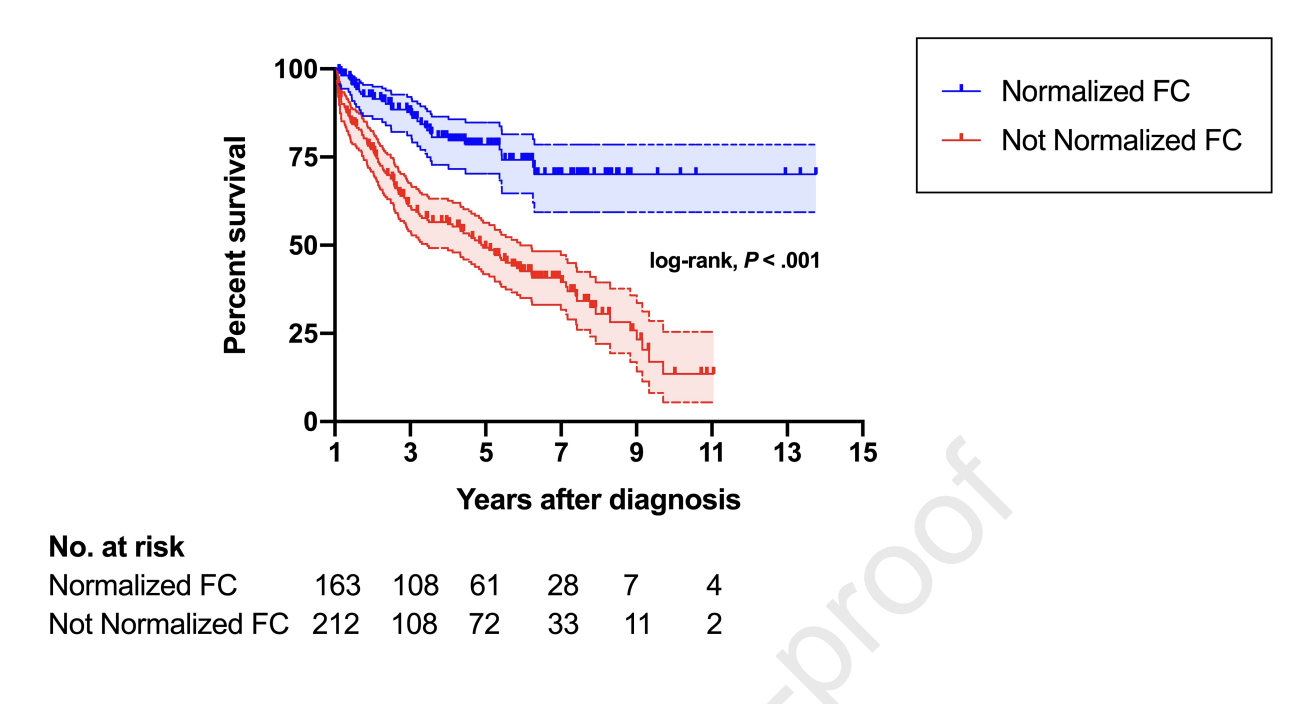
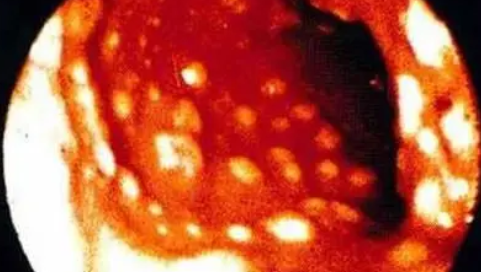
图:粪钙卫蛋白水平变化对于疾病复发的影响
通过本项回顾性研究,作者证实CD患者在被诊断后 12 个月内 FC 正常化与 CD 进展风险降低相关。
原始出处:
Nikolas Plevris. Et al. Normalization of Fecal Calprotectin Within 12 Months of Diagnosis Is Associated With Reduced Risk of Disease Progression in Patients With Crohn’s Disease. Clinical Gastroenterology and Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#风险降低#
24
#AST#
31
#GAS#
30
#疾病进展#
32
#Gastroenterol#
35
#Gastroenterology#
0