Eur Urol Oncol: 免疫环境和分化特征可预测膀胱癌结局
2022-04-01 AlexYang MedSci原创
研究确定了免疫细胞亚群和癌细胞内在特征是否与BC的结局和对一线化疗的反应有关。
膀胱癌(BC)是一种高度分子异质性疾病,每个癌细胞的表型受多种癌细胞内源性和外源性特征的影响,这些特征可能驱动疾病的发展和治疗耐药性。改进对BC患者的风险评估对于优化临床管理非常重要。近日,来自丹麦奥胡斯大学等单位的研究人员研究确定了免疫细胞亚群和癌细胞内在特征是否与BC的结局和对一线化疗的反应有关。相关研究结果发表在《EUROPEAN UROLOGY ONCOLOGY》期刊上。
研究人员使用多重免疫荧光(CD3、CD8、FOXP3、CD20、CD68、CD163和MHC-I)和免疫组化(pancytokeratin、CK5/6、GATA3、PD-1和PD-L1)对785名BC患者(Ta-T4b期)的原发肿瘤组织进行了检测,并通过数字图像分析对肿瘤的癌细胞和基质部分的染色结果进行了量化。
研究的主要终点是无进展生存期、无复发生存期和对一线化疗的反应。研究人员使用最大选择等级统计和ROC对每个主要终点的调查标记物的最佳截止值进行了估计,并采用Cox回归分析法进行时间-事件分析。
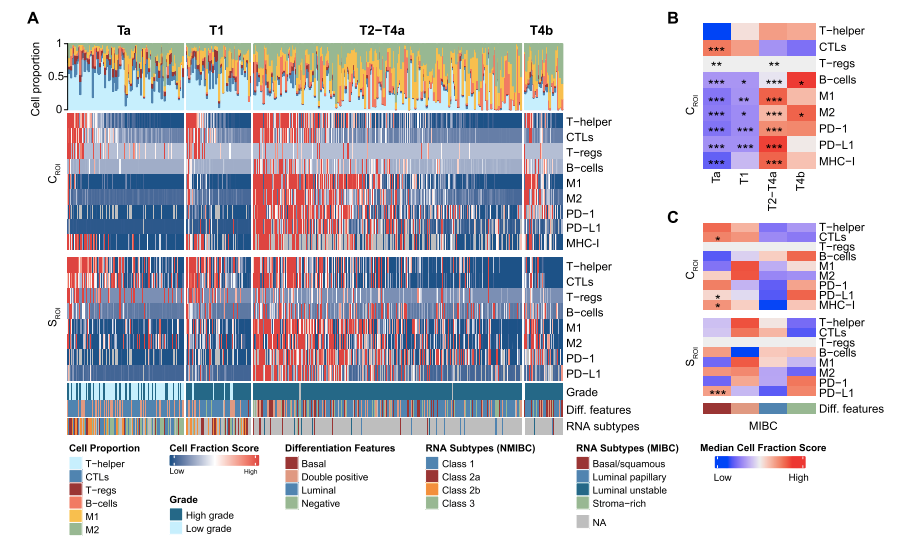
图1 与阶段和分化特征相关的免疫亚群和免疫逃避标记物
结果显示,几个免疫亚群与临床结果独立相关。特别是PD-1和PD-L1的高表达与非肌肉浸润性肿瘤的复发和进展风险增加独立相关,但与肌肉浸润性肿瘤的复发风险较低。此外,他们观察到具有基底分化特征的患者对一线化疗反应的可能性较低。最后,与单独的临床风险因素相比,将临床风险因素与最明显的预后指标相结合的模型提高了对非肌肉浸润性BC进展和肌肉浸润性BC复发的预测准确性。组织芯片的使用和较长的纳入期是本研究的局限性。
综上所述,免疫细胞亚群和癌细胞内在特征与BC的不同临床结果有关。免疫细胞在癌症的发展和治疗结果中起着重要作用。特异性免疫细胞浸润和肿瘤中与免疫逃避相关的标记物的存在可以预测膀胱癌的临床结局。
原始出处:
Ann Taber , Frederik Prip , Philippe Lamy et al. Immune Contexture and Differentiation Features Predict Outcome in Bladder Cancer. Eur Urol Oncol. Feb 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
30
学习了
63
学习一下
64
学习学习了
54
认真学习~~
63
认真学习了
57