初始安立生坦联合5型磷酸二酯酶抑制剂对重度肺动脉高压患者右心室肺动脉耦合的超声心动图评估
2022-05-24 刘少飞 MedSci原创
肺动脉高压 (PAH) 是一种严重的临床综合征,其特征是肺血管阻力增加,导致右心衰竭和死亡。本研究的目的研究初始安立生坦联合 PDE5i 联合治疗对重度 PAH 患者 RVPAC 的影响和临床相关性。
研究背景:
安利生坦和5型磷酸二酯酶抑制剂(PDE5i)已被批准用于治疗肺动脉高压(PAH)患者。PAH 症状和结果的主要预后因素与 RV 功能有关。然而,仅评估 RV 功能对 RV 适应和慢性容量超负荷的了解有限,并且没有考虑肺循环的影响。基于右室功能与其血管循环匹配的右心室肺动脉耦合(RVPAC)可以早期、准确地反映右室功能超负荷的状态。评估 RVPAC 的金标准是收缩末期弹性与肺动脉弹性的比值 (Ees/Ea),已通过侵入性右心导管 (RHC) 进行评估。理想情况下,适应性 RV 患者在静息状态下保持耦合。只有在压力过载的后期才会发生解耦。超声心动图右心室肺动脉耦合(RVPAC)已被证明是评估PAH患者预测结果的有效的无创和替代测量方法。
研究目的:
研究初始安利生坦加PDE5i联合治疗对严重PAH患者RVPAC的影响和临床相关因素。
研究方法和结果:
我们回顾性地研究和分析了27名重度PAH患者在初始联合治疗前后6个月的综合临床数据、血流动力学和超声心动图。与基线相比,观察到RVPAC比率的显著改善,包括RVFAC/PASP(0.31±0.10 vs. 0.44±0.15%/mmHg,P<0.001),TAPSE/PASP(0. 15 ± 0.05 vs. 0.21 ± 0.06 mm/mmHg,p = 0.001),S'/PASP(0.10 ± 0.03 vs. 0.14 ± 0.05 cm/s∙mmHg,p = 0.001),以及RVSV/RVESV(0.79 ± 0.22 vs. 1.02 ± 0.20,p < 0.001)。功能状态指数[世界卫生组织功能分类(WHO-FC)和6分钟步行距离(6MWD)以及N-末端B型钠尿酸肽(NT-proBNP)水平]显示出明显改善。基线和6-12个月的随访期间,右心导管检查(RHC)对血流动力学测量的评价是sPAP(96±22 vs. 86±24 mmHg,p = 0.002),mPAP(64±18 vs. 56±17 mmHg,p < 0.001)和TPVR(17.3±6.7 vs. 12.1±5.4 WU,p = 0.001)。同时,观察到RVPAC比率和NT-proBNP水平与WHO-FC和6MWD之间的显著关联。
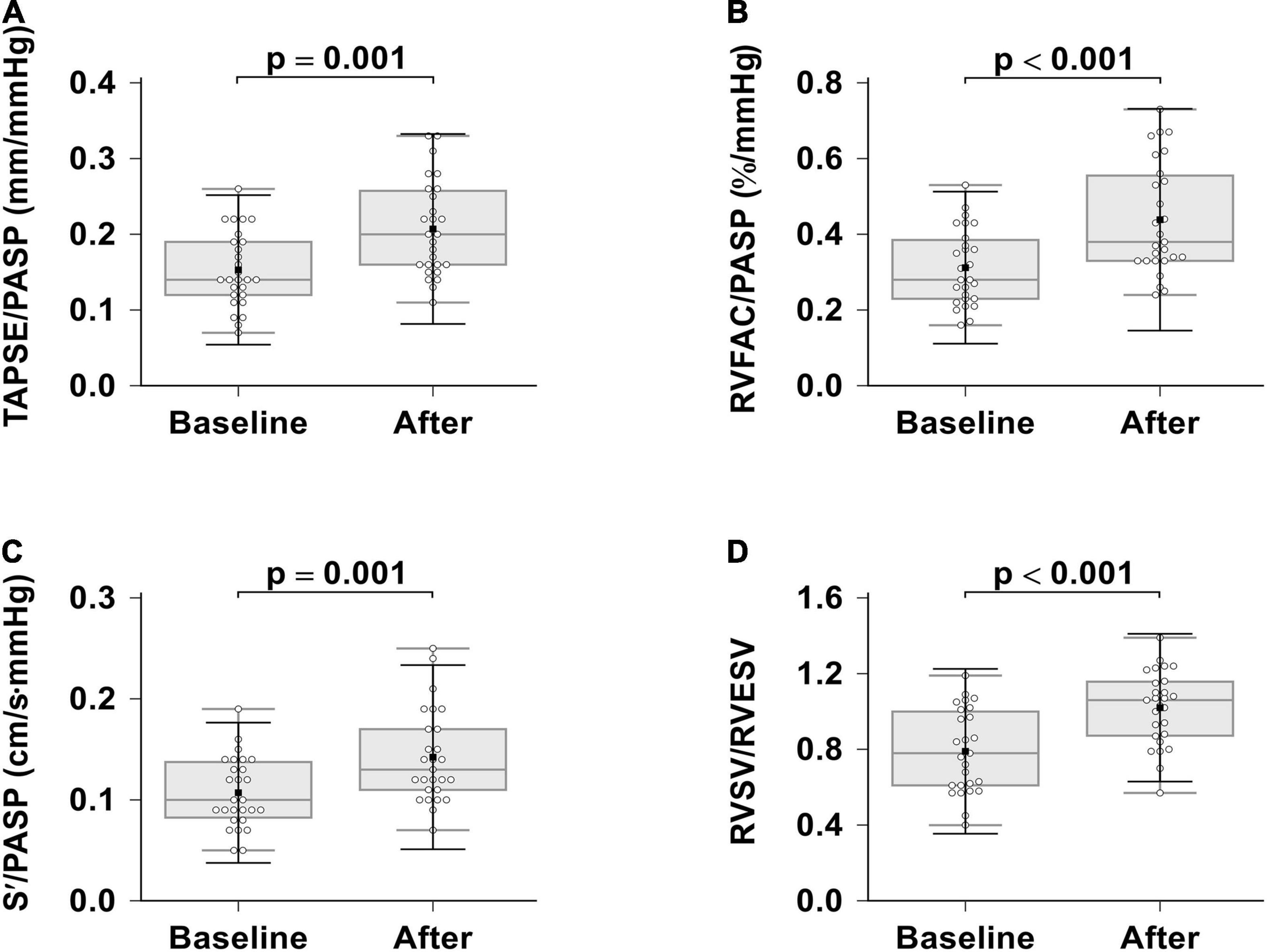
图 1 .安立生坦联合 PDE-5i 联合治疗对右心室肺动脉耦合的影响。(A) TAPSE/PASP;(B) RVFAC/PASP;(C) S'/PASP;(D) RVSV/RVESV。TAPSE,三尖瓣环平面收缩偏移;RVFAC,右心室部分面积变化,S',三尖瓣环收缩速度;PASP、肺动脉收缩压、RVEF、右心室射血分数;RVESV,右心室收缩末期容积;RVSV,右心室每搏输出量。
研究结论:
安利生坦加PDE-5i联合治疗使严重PAH的RVPAC得到明显改善。这些发现提供了对安立生坦加 PDE-5i 联合治疗的血流动力学和 RV 影响的深入了解。更重要的是,RVPAC 与已知的 PAH 预后标志物相关。RVPAC 可能是 RV 功能和临床改善响应联合治疗的准确无创和敏感标志物。综合考虑患者数量少等多重因素,结论慎重。因此,未来的前瞻性研究需要确定联合治疗是否或多长时间可以优化 RV 逆转重塑,并根据严重 PAH 患者的长期随访评估治疗结果,为临床实践提供进一步的见解。
参考文献:
Lan WF, Deng Y, Wei B, Huang K, Dai P, Xie SS, Wu DD. Echocardiographic Evaluation of Initial Ambrisentan Plus Phosphodiesterase Type 5 Inhibitor on Right Ventricular Pulmonary Artery Coupling in Severe Pulmonary Arterial Hypertension Patients. Front Cardiovasc Med. 2022 May 3;9:843606. doi: 10.3389/fcvm.2022.843606. PMID: 35592406; PMCID: PMC9113403.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
35
#抑制剂#
71
#心动图#
56
#5型磷酸二酯酶抑制剂#
40
#肺动脉高压患者#
40
精彩评论,需要您登录查看
27
#右心室#
44