Oncogene:ApoC1能够促进透明细胞肾细胞癌的转移
2020-09-13 AlexYang MedSci原创
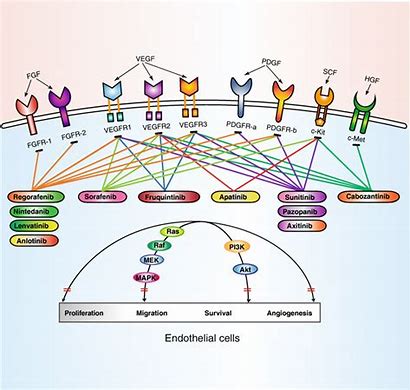
透明细胞肾细胞癌(ccRCC)是最常见的肾癌,且诊断经常为晚期。即使经过适当的治疗,也容易发生不可预测的转移。抗血管生成治疗是转移性ccRCC最有效的治疗方法。因此,探索抑制血管生成和转移的新方法有可
透明细胞肾细胞癌(ccRCC)是最常见的肾癌,且诊断经常为晚期。即使经过适当的治疗,也容易发生不可预测的转移。抗血管生成治疗是转移性ccRCC最有效的治疗方法。因此,探索抑制血管生成和转移的新方法有可能为ccRCC带来更好的治疗方案。
在所有类型的癌症中,肾癌样本再Oncomine数据库中ApoC1的上调幅度最大,且ApoC1的表达增加伴随着ccRCC的进展。在ccRCC患者中,高水平的ApoC1蛋白与较差的生存时间密切相关。更多的是,ApoC1在高侵袭性ccRCC细胞中的表达量比低侵袭性ccRCC细胞高。此外,ApoC1能够通过EMT途径促进ccRCC细胞的转移,ApoC1的失却能够减弱这些作用。ApoC1作为一种新型的促转移因子,能促进STAT3的激活,增强ccRCC细胞的转移。同时,外泌体中的ApoC1能够从ccRCC细胞转移到血管内皮细胞,通过激活STAT3促进ccRCC细胞的转移。
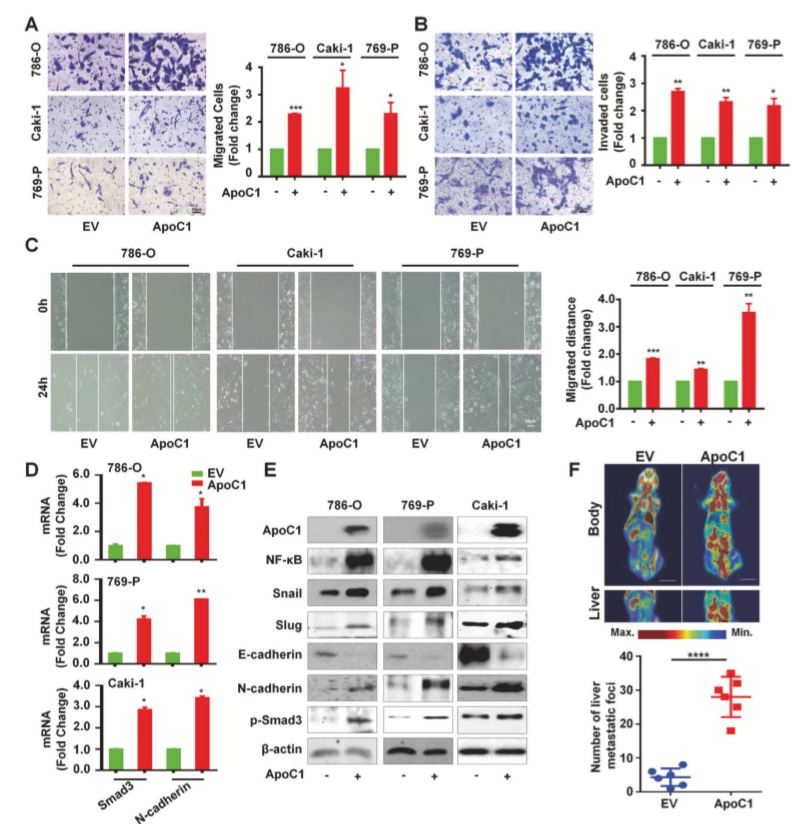
ApoC1促进ccRCC的转移
最后,研究人员指出,由ApoC1驱动的ccRCC细胞的转移潜能被DPP-4抑制剂所抑制。他们的研究不仅鉴定了在ccRCC转移中新的ApoC1-STAT3通路,也为未来预测和治疗转移性ccRCC的新策略的探索提供了方向。
原始出处:
Yang-ling Li, Lin-wen Wu, Ling-hui Zeng et al. ApoC1 promotes the metastasis of clear cell renal cell carcinoma via activation of STAT3. Oncogene. August 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#细胞癌#
32
#Gene#
44
#Oncogene#
49
ApoC1
88
打卡学习
84