JACC:双重血管紧张素受体减轻多柔比星诱导的心脏毒性作用
2021-01-04 MedSci原创 MedSci原创
与标准血管紧张素受体阻滞剂治疗相比,在DOX诱导的进行性心脏毒性的啮齿动物模型中,Sac/Val对左心室重塑和功能障碍提供了更大的保护。
根据美国心力衰竭学会(HFSA)第22届年会上发表的一项研究,脑啡肽酶抑制剂Sacubitril(沙库必曲)/ 血管紧张素Ⅱ受体拮抗剂Valsartan(缬沙坦)即LCZ696(Entresto),可以使心衰患者的射血分数(HFrEF)迅速恢复。美国FDA于2015年7月7日批准诺华公司的Sacubitril / Valsartan (Sac/Val)片剂上市,用于射血分数降低的慢性心力衰竭(NYHA心功能Ⅱ~Ⅳ级)患者,以降低心力衰竭相关心血管死亡和住院风险。

已知多柔比星(DOX)部分通过激活基质金属蛋白酶(MMPs)诱导心脏毒性。Sac/Val在心肌梗死的临床前模型和心力衰竭患者中,比肾素-血管紧张素-醛固酮抑制剂(RAAS)的心脏保护作用更强。因此,在DOX诱导的进行性心脏毒性的啮齿动物模型中,Sac/Val比Val更具心脏保护作用,这种益处是否与MMP激活的调节有关呢?
为此,来自美国耶鲁大学医学院的研究团队进行了相关的研究,探讨Sac/Val治疗蒽环类药物引起的心脏毒性的疗效。结果发表在最新的JACC杂志上。
雄性Wistar大鼠在3周内腹腔注射DOX(累计15mg/kg)或生理盐水。第一次注射后,对照组动物每天用水灌胃(n = 25),而DOX治疗的动物每天用水(n = 25)、Val(31 mg/kg;n = 25)或Sac/Val(68 mg/kg;n = 25),持续4或6周灌胃。在基线、DOX注射后4周和6周分别进行超声心动图检查。此外,在上述时间点使用99mTc-RP805评估心肌MMP活性,并通过组织学评估动物的心脏毒性严重程度。
结果显示,DOX和DOX + Val大鼠的左心室射血分数在6周时下降了10%(Ps均 <0.05),而DOX + Sac/Val大鼠的下降没有上述明显。与时间匹配的对照动物相比,6周时DOX注射大鼠MMP活性增加了76%,在DOX+Val大鼠也增加(36%;p = 0.051),但DOX + Sac/Val大鼠的MMP活性没有明显差异。组织学检查提示,两种疗法都减轻了心脏细胞毒性和纤维化程度(p <0.05)。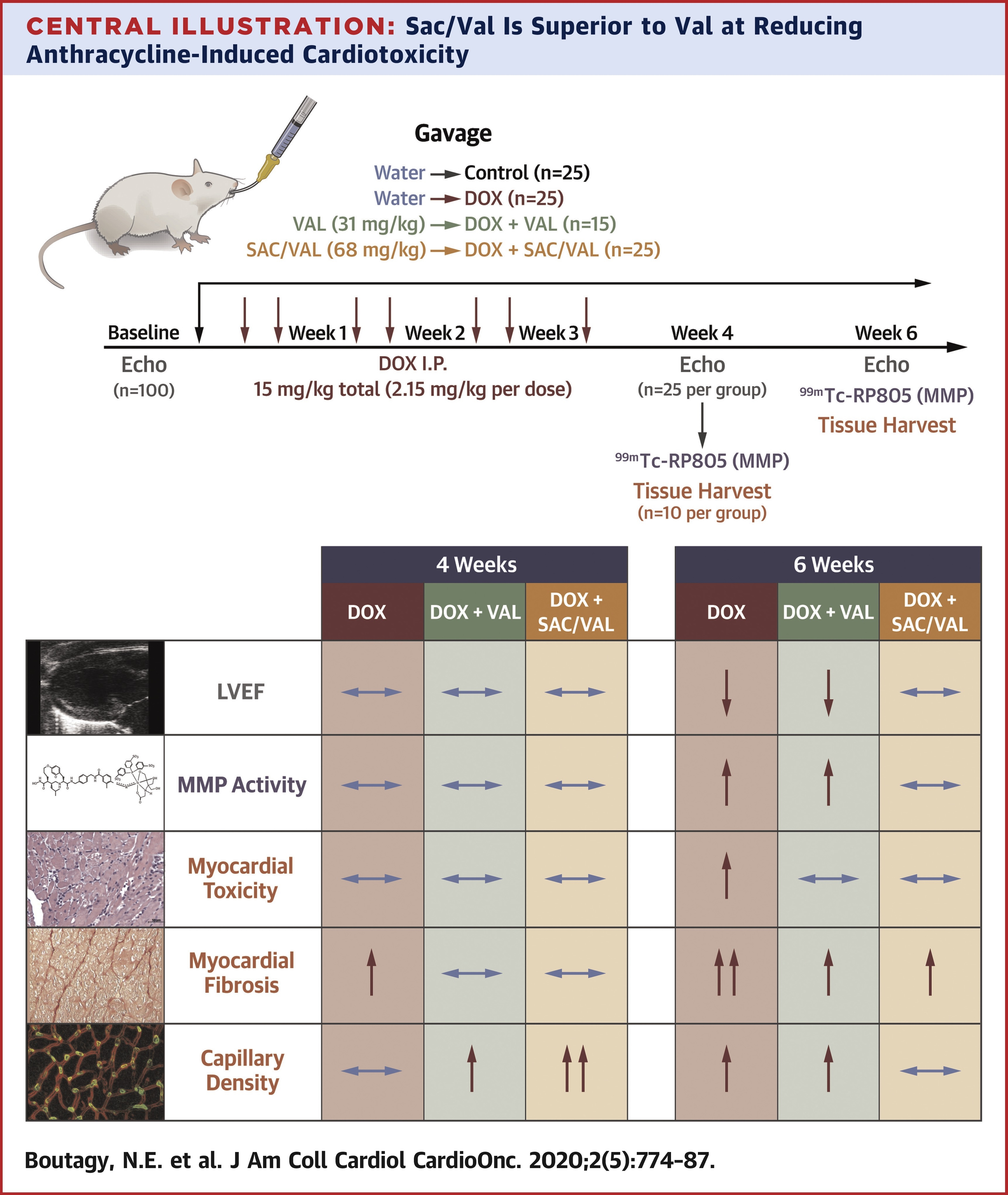
上述结果提示,与标准血管紧张素受体阻滞剂治疗相比,在DOX诱导的进行性心脏毒性的啮齿动物模型中,Sac/Val对左心室重塑和功能障碍提供了更大的保护。
参考文献:
Nabil E.B. et al. Dual Angiotensin Receptor-Neprilysin Inhibition With Sacubitril/Valsartan Attenuates Systolic Dysfunction in Experimental Doxorubicin-Induced Cardiotoxicity. J Am Coll Cardiol CardioOnc. 2020 Dec, 2 (5) 774–787.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#毒性作用#
46
#JACC#
31
AT1受体被阻断后,反馈性地增加血浆肾素水平,引起血浆Ang II浓度升高。但由于AT1受体已被断,这些反馈性作用难以表现。但是血浆中升高的AngII通过激活AT2受体,可激活缓激NO途径,产生舒血管、降低血压等效应,有益于高血压与心力衰竭的治疗.
74
学习了!
87
#多柔比星#
128
#ACC#
31
#血管紧张素#
37
学习了
86
#心血管#
129