ICM:危重病内科患者药物预防 VTE 的持续时间
2019-06-05 杨中华 脑血管病及重症文献导读
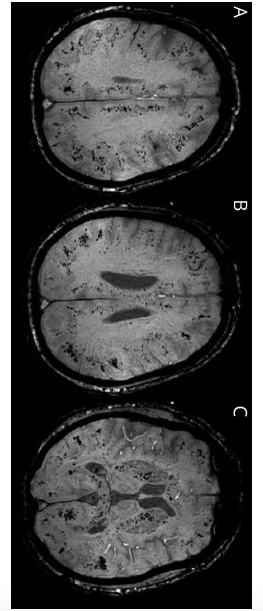
静脉血栓栓塞(Venous thromboembolism,VTE)是危重病的常见并发症,是一种可预防的疾病。在 ICU 中,多种危险因素共同促成了 Vinchow 三联症(高凝性、静脉内膜完整性的破坏、静脉血流瘀滞)。首先,危重病患者长时间不能活动,心肺衰竭,腹腔内高压,或使用了神经肌肉阻滞剂,这些皆会有可能导致血液淤滞。其次,一些因素比如脓毒症、炎症、慢性肾病、输血和使用促红细胞生成素刺激剂等
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#危重病#
27
学习了
83
学习了,谢谢分享
82
#持续时间#
26
#药物预防#
34