Front Neurosci:六味地黄汤通过肠道-脑轴调节脂质代谢和氧化应激,减轻衰老小鼠的认知功能障碍
2022-08-17 紫菀款冬 MedSci原创
从微生物群肠脑轴的角度解释六味地黄汤缓解与衰老相关的认知功能障碍的机制。
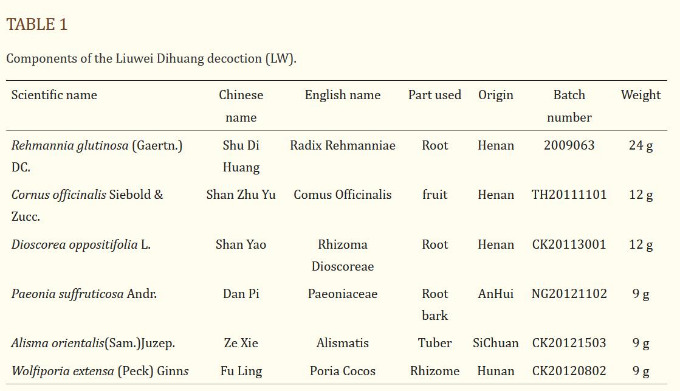
背景:衰老是认知功能障碍的重要原因。六味地黄汤(LW)是一种常用的中药配方,在中国被广泛用于治疗与衰老相关的疾病。此前,LW被证实能有效延长老年小鼠的寿命并减少氧化应激。然而LW的潜在机制尚不清楚。
目的:从微生物群肠脑轴的角度解释LW缓解与衰老相关的认知功能障碍的机制。
方法:60只C57BL/6小鼠(n=60)随机分为5组:对照组、模型组、维生素E(阳性对照组)、低剂量LW和高剂量LW组(n=12)。
除对照组外,其余各组小鼠皮下注射D-半乳糖诱导衰老模型。通过水迷宫试验、电子显微镜观察、16S rRNA测序、LC-MS和GC-MS代谢组学结合以及ELISA评估LW的抗衰老作用。
结果:LW能改善衰老小鼠的认知功能障碍和海马突触超微结构损伤。此外,LW降低了衰老小鼠中蛋白质细菌的丰度,增加了肠道微生物群的多样性。
代谢组学分析表明,LW处理与14种代谢物的丰度显著差异相关,这些代谢物主要富集于apelin信号、鞘脂代谢、甘油磷脂和其他代谢途径。
LW可影响衰老小鼠的脂质代谢和氧化应激——升高载脂蛋白E和脂联素含量,降低游离脂肪酸含量;降低MDA含量,增强SOD和GSH-Px活性。
该研究还发现LW调节的微生物种群,如蛋白细菌和纤维细菌,与脂质代谢、氧化应激和海马代谢产物有潜在的关系。
结论:LW通过恢复肠道-脑轴微生物群的动态平衡来调节脂质代谢和氧化应激,从而改善衰老小鼠的认知功能。此外,LW诱导的变形杆菌和纤维杆菌的变化可能与脂质代谢和氧化应激有关,值得进一步研究。
文献来源:
Liu B, Chen B, Yi J, et al. Liuwei Dihuang Decoction Alleviates Cognitive Dysfunction in Mice With D-Galactose-Induced Aging by Regulating Lipid Metabolism and Oxidative Stress via the Microbiota-Gut-Brain Axis. Front Neurosci. 2022;16:949298. Published 2022 Jul 1. doi:10.3389/fnins.2022.949298
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#脂质代谢#
61
#ROS#
74
#功能障碍#
77
#应激#
54