实用汇总:6张表牢记心脏超声正常值
2021-12-09 MedSci原创 MedSci原创
心脏超声,相当于医生的“透视眼”,能动态的显示心脏内结构、心脏的搏动和血液流动的检查,不需要开胸,就可以看到心脏的大小、内部结构和运动情况等。
心脏超声,相当于医生的“透视眼”,能动态的显示心脏内结构、心脏的搏动和血液流动的检查,不需要开胸,就可以看到心脏的大小、内部结构和运动情况等。
而心脏超声是心内科较常用的一项辅助检查手段,主要用于各种先心病、心脏瓣膜病的诊断,心功能评估以及各种心肌病,心包疾病的诊断等。心脏超声报告看起来很复杂,但是掌握了这几个核心的指标,就可化繁为简。本文整理并汇总了心脏超声各项指标的正常值,希望临床医生能更加轻松的理解超声报告。
首先,我们要熟悉关键的指标,主要包括心脏四个腔室的大小、容积及室壁厚度,主动脉和肺动脉内径、二尖瓣、主动脉瓣及肺动脉瓣的流速,左室射血分数LVEF等等各项指标。
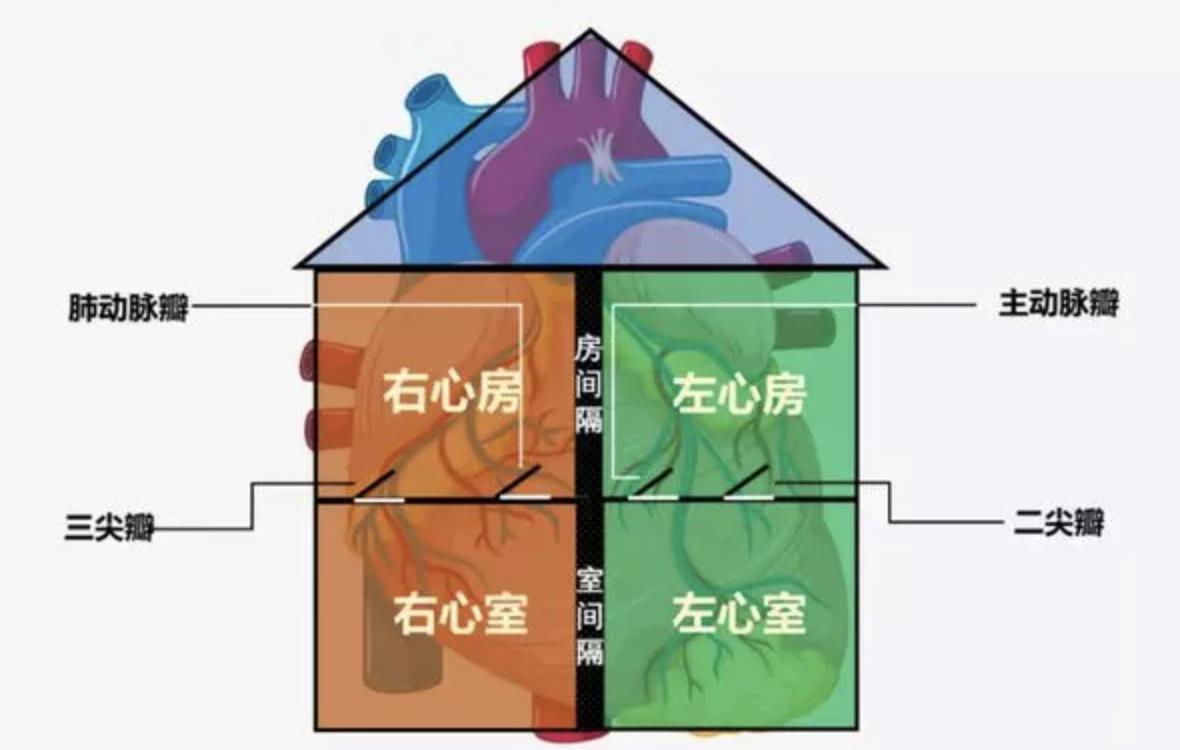
图片来源:医阶
1、腔室大小
心腔的大小,通常以心腔内径作为衡量指标,主要观察的是左右心房及左右心室四个腔。如果超出正常值范围,需要及时查明病因。

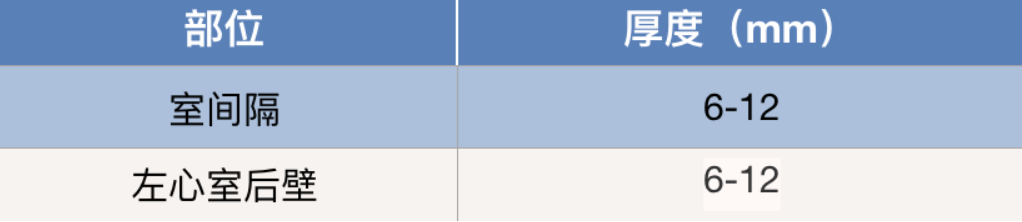
2、室壁厚度
室壁的厚度一般主要检测室内隔及左心室后壁厚度。如果测得值提示心肌变厚,则提示左心室可能长期存在较高的压力。当然,也可能是心肌自身原发性增厚,如肥厚型心肌病等。
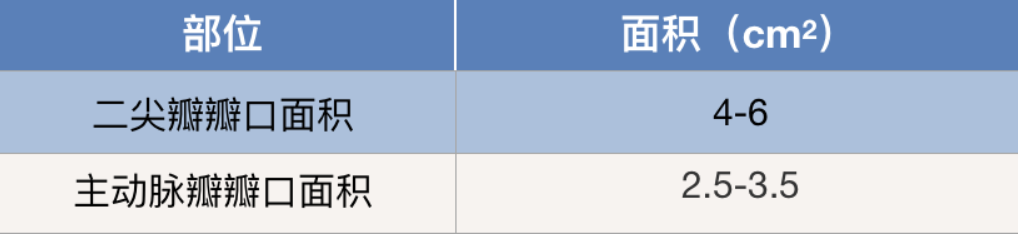
3、瓣膜大小
瓣膜大小主要检测二尖瓣及主动脉瓣口面积。当瓣口面积小于正常值时,考虑存在狭窄情况,需要结合瓣膜口两侧压差判断。当瓣口面积变大时,往往合并心腔变大。
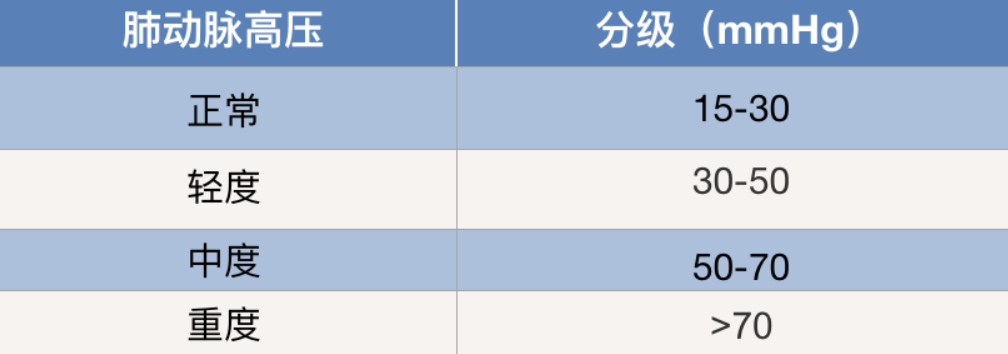
4、右心室承受阻力
右心室承受阻力常常用的指标为肺动脉压力。超过正常即考虑有肺动脉高压,根据其增高程度的不同分为轻度、中度及重度。
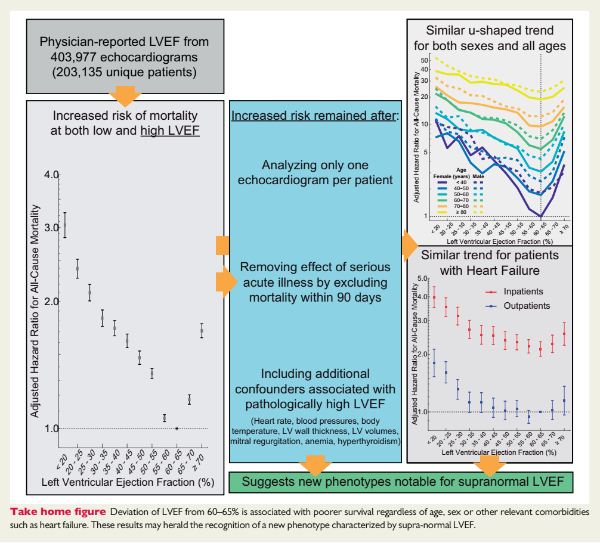
5、心脏排血能力
心脏排血能力常检测左心室射血分数(LVEF),主要反映左心室收缩功能。若LVEF数值降低,可考虑存在不同程度的心力衰竭。

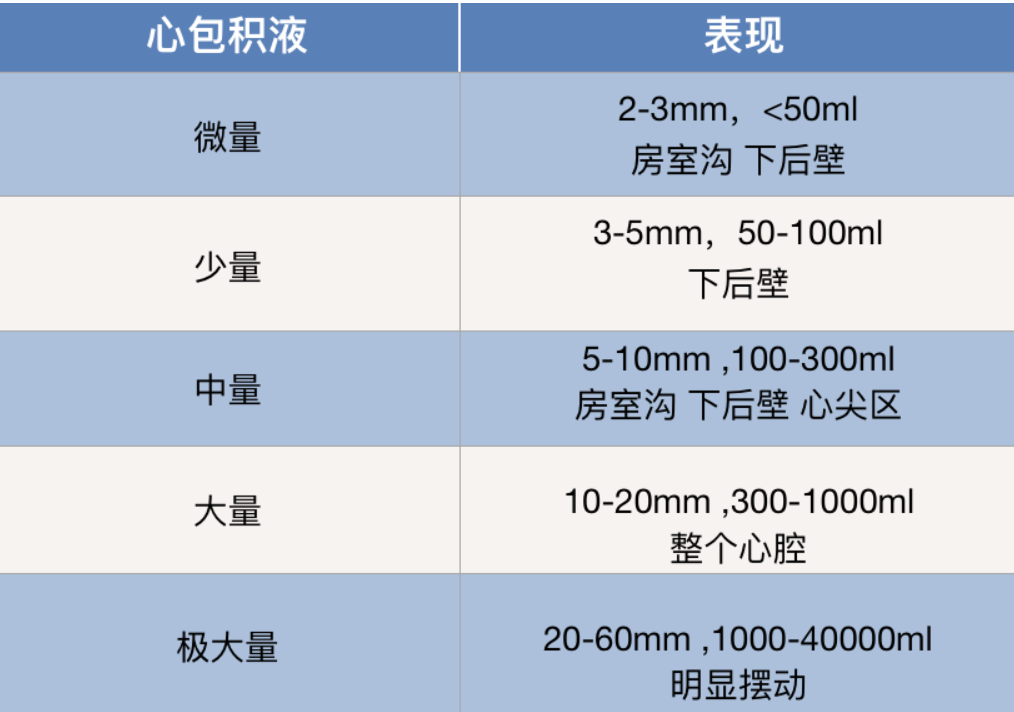
6、心包积液
超声多以观测到的液体深度(液深)来表示,根据液深可以估算液体的容量。如果报告中出现心包积液,很可能是感染、肿瘤或免疫性疾病等导致,需要找出背后的元凶。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
63
#心脏超声#
45
学习
66
学习
73
学习
90