肝癌是我国最常见的消化道癌症之一,我国每年约11万人死于肝癌,占全世界肝癌死亡人数的45%。胆管癌是发生于胆管系统的恶性肿瘤,是比较常见的恶性肿瘤疾病。这两种疾病发病率高,较难治疗。近日,西班牙科学家们发现了一种蛋白质,能够抑制肝癌和胆管癌的发展。

研究人员已经找到了一种机制,能够控制肝癌的发展。这一研究发表在《美国国家科学院院刊》(PNAS)杂志上。由西班牙抗癌协会提供部分资助。这项研究发现了一种蛋白质,当它被阻断时,可以显着降低胆管癌的影响和进展。
这项工作之所以成为可能,是因为中国科学院计算机网络信息中心(CNIC)的研究人员开发了一种动物模型,胆汁酸产生的改变已被证明是导致这种类型肿瘤的原因。
肝癌是全球第五大最常见的癌症,也是导致癌症相关死亡的第二大主要原因。胆管癌是第二常见的肝癌,开始于胆管,临床上无症状发展。由于没有早期标志物,大多数患者被诊断为晚期,并因癌症扩散或转移而死亡。
在这项由瓜达卢佩·萨比奥(Guadalupe Sabio)、阿方索·莫拉(Alfonso Mora)和罗杰·J·戴维斯(Roger·J·Davis)领导的研究中,培育了肝脏不含JNK1和JNK2蛋白的小鼠。萨比奥博士解释说,“当我们吃得过多的时候,这些蛋白质就会被激活,并在一定程度上导致肝脏中储存过多的脂肪(即脂肪肝或脂肪变性)。并导致胰岛素的抵抗,因此,这些蛋白质对肥胖和糖尿病的研究非常重要。”
研究人员还发现,这两种蛋白质控制肝脏中胆汁酸的产生,而胆汁酸对脂肪的适当消化和脂溶性维生素(A、D、E和K)的吸收至关重要。肝脏中JNK1和JNK2的缺乏会导致负责代谢胆固醇和胆汁酸的酶发生变化,在被分析的小鼠中,可以看到血液中胆汁酸过多。
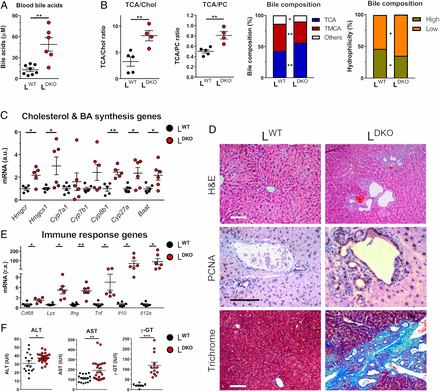
肝脏JNK缺乏会改变胆汁酸的产生并引起胆汁淤积
研究人员解释说,随着时间的推移,胆汁酸的积累对肝脏有“毒性作用”。胆管开始过度增生,触发多种胆管癌的形成,临床标志物与这类癌症的患者非常相似。事实上这是他们第一次在小鼠模型中发现胆管癌患者标志物的增加。这表明这些小鼠可以为评估新的胆管癌治疗方法提供新的线索。
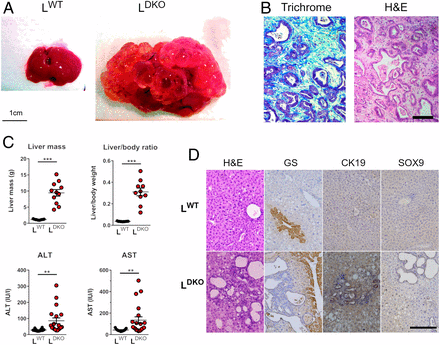
肝JNK缺乏进展为胆管癌
这一模型使CNIC的研究人员与美国麻省大学医学院罗杰·J·戴维斯实验室合作,找到了一种在肿瘤发生过程中起关键作用的蛋白质,PPAR。该蛋白调节胆汁酸和肝脂的代谢。
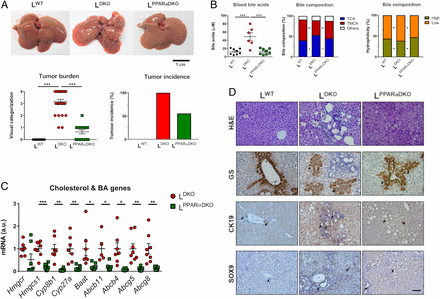
PPAR缺陷可降低肝脏JNK缺陷引起的肝癌
虽然还不知道这些数据是否可以推断到人类患者,但事实上,第一个动物模型的存在将允许研究一种仍只能在晚期诊断的肿瘤,那时已经发生了转移。
早期的研究表明JNK阻断可以防止肝脏脂肪变性的发展。这就是为什么针对这些蛋白质抑制剂的各种临床试验已经启动。研究人员认为,这些新发现为这些药物敲响了警钟。
尽管这项工作只在老鼠身上进行了试验,但研究人员指出,我们必须小心谨慎,对接受这些新药治疗的病人肝脏的结果保持警惕。
原始出处:Elisa Manieri, Cintia Folgueira, María Elena Rodríguez, et al. JNK-mediated disruption of bile acid homeostasis promotes intrahepatic cholangiocarcinoma. PNAS. June 29, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阻断#
37
#新突破#
36
#PNAS#
36
阻遏蛋白
104
#胆管#
26
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
50