Tonetti教授发文,十年随机对照试验结果为重度牙周炎无望牙的“拔与留”提供原则性指导
2021-04-10 MedSci原创 MedSci原创
牙周组织再生可以改变牙齿的预后,对于严重骨缺损的牙齿,牙周组织再生或可使其免除拔除的命运。近日,Tonetti教授发文报道了其领导的为期10年的随机对照临床试验的结果,该试验纳入了牙周组织丧失至根尖甚
牙周组织再生可以改变牙齿的预后,对于严重骨缺损的牙齿,牙周组织再生或可使其免除拔除的命运。近日,Tonetti教授发文报道了其领导的为期10年的随机对照临床试验的结果,该试验纳入了牙周组织丧失至根尖甚至超出根尖范围的牙齿,比较了牙周组织再生(PR)与拔除与种植修复(TER)的临床、患者报告和经济结果,已发表于J Clin Periodontol。
研究纳入了50名III期或IV期牙周炎受试者,附着丧失至或超出根尖区,随机分配接受PR或TER(种植体或牙支持固定桥)修复。受试者每3个月进行一次严格的牙周支持护理,每年检查一次。进行生存和复发分析。
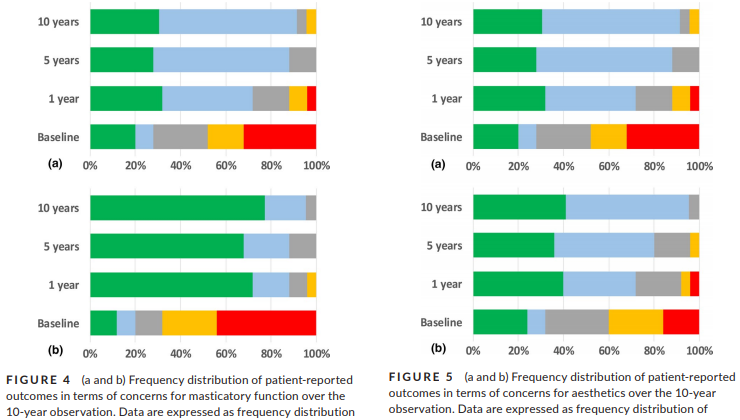
结果显示,PR组和TER组的生存率分别为88%和100%。无并发症,生存期无显著差异:PR为6.7-9.1年,TER为7.3-9.1年(P=0.788)。在PR组中,观察到的10年附着增加为7.3±2.3mm,残余探诊深度为3.4±0.8mm。

复发分析显示,在整个10年随访期间,与TER组相比,PR组治疗费用的95%置信区间显著降低。两组患者报告的结果和口腔健康相关的生活质量测量结果均有所改善。
综上所述,该试验结果表明,牙周组织再生可以改变无望牙的预后,是一种成本较低的拔牙和种植牙的替代治疗方法。虽然治疗的复杂性限制了在最复杂病例中的广泛应用,但为PR在深部骨内缺损中的治疗优势提供了有力的原则性证明。
原始出处:
Pierpaolo Cortellini, et al., Periodontal regeneration versus extraction and dental implant or prosthetic replacement of teeth severely compromised by attachment loss to the apex: A randomized controlled clinical trial reporting 10-year outcomes, survival analysis and mean cumulative cost of recurrence. J Clin Periodontol. 2020 Jun;47(6):768-776. doi: 10.1111/jcpe.13289.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#NET#
24
#对照试验#
40
#重度牙周炎#
32
#对照#
33
#随机对照试验#
39
#牙周#
40
高质量研究,读起来真爽,谢谢梅斯
44
好文章!
63