Sci Rep:乳头状肾细胞癌亚型对肿瘤治疗效果的影响
2020-12-16 AlexYang MedSci原创
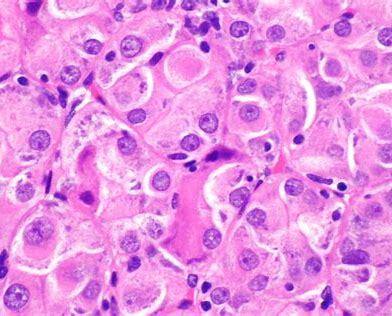
最近,有研究人员比较了I型和II型乳头状肾细胞癌(PRCC)的临床病理特征和预后,并调查了PRCC的亚型是否会影响肿瘤学结果。
最近,有研究人员比较了I型和II型乳头状肾细胞癌(PRCC)的临床病理特征和预后,并调查了PRCC的亚型是否会影响肿瘤学结果。

研究共招募了102名PRCC患者,其中I型PRCC有42名,II型PRCC有60名,并评价了患者的临床病理特征和肿瘤学结果。研究发现,II型病例的WHO/ISUP分级(P<0.001)、T(P=0.003)、N(P=0.010)期和分期分组(P=0.011)均高于I型。在中位值为61.4个月的随访期内,I型的1年癌症特异性生存率(CSS)为100%,5年CSS为95.2%;II型的1年CSS为96.2%,5年CSS为75.7%。单变量分析表明,亚型、症状、TNM、分期分组、WHO/ISUP分级和手术方法似乎影响了PRCC患者的预后。然而,多变量分析显示,只有分期分组是独立的风险因素。在对分期分组因素进行调整分析后,局部I型和II型PRCC组之间的CSS(P=0.214)和PFS(P=0.190)没有统计学显著差异。

I型和Ⅱ型乳头状肾细胞肿瘤的无进展生存比较
最后,研究人员指出,与I型PRCC相比,II型的病理T、N期和WHO/ISUP分级更高。然而,分期分组能够产生肿瘤学结果的巨大差异,而非PRCC的亚型。
原始出处:
Honghong Pan, Liefu Ye, Qingguo Zhu et al. The effect of the papillary renal cell carcinoma subtype on oncological outcomes. Sci Rep. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#乳头状#
52
#细胞癌#
38
阿昔联合PD-1进展咋搞
85
#治疗效果#
38
#肿瘤治疗#
42
学习了,谢谢分享
78
谢谢梅斯提供这么好的信息,学到很多
53
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
50
分期分组
92