Cancers (Basel):局部前列腺癌患者经尿道前列腺切除术后的前列腺特异性抗原变化的预测作用
2021-01-12 AlexYang MedSci原创
关于局部前列腺癌(PC),哪些患者适合保守治疗仍是个问题。一些局部PC患者是因泌尿系统症状而接受经尿道前列腺切除术(TURP)中偶然发现的。TURP通常会影响前列腺特异性抗原(PSA)的水平。
关于局部前列腺癌(PC),哪些患者适合保守治疗仍是个问题。一些局部PC患者是因泌尿系统症状而接受经尿道前列腺切除术(TURP)中偶然发现的。TURP通常会影响前列腺特异性抗原(PSA)的水平。
最近,有研究人员调查了TURP后PSA水平的变化是否对局部PC具有预测价值。他们回顾性地审查了846名早期PC患者的临床资料,这些患者因泌尿系统症状进行了TURP。结果表明,846名患者中有687名患者的TURP样本中有肿瘤累及,362名患者进行了TURP后的PSA评估。数据显示,除诊断时GS和PSA水平较低外,TURP样本中肿瘤累及率≤5%、TURP后PSA下降幅度较大(≥68%)以及TURP后PSA≤4与较好的无进展生存期(PFS)显著相关。生存分析表明,在中、高风险组中,加入前列腺导向局部治疗可显著改善PFS,但在低风险组中则没有。更多的是,在中风险组中,局部治疗仅对TURP后PSA>4 ng/mL或TURP后PSA降低<68%的相关患者具有PFS改善效果。他们还发现,无论TURP前PSA如何,局部治疗对TURP后≤4 ng/mL患者的PFS无明显改善。
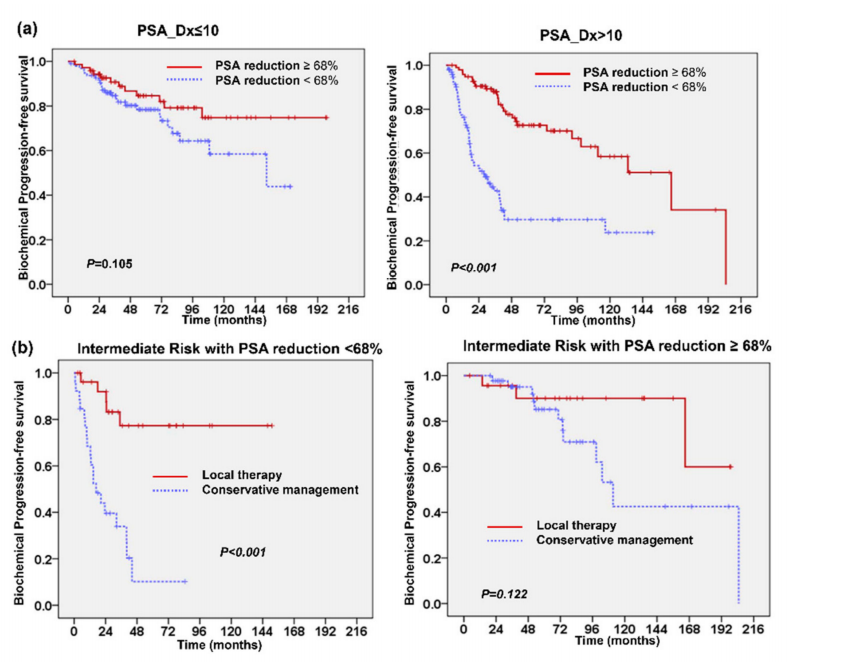
TRUP后PSA减少于局部前列腺癌患者的临床结果相关
最后,研究人员指出,对于TURP后PSA下降幅度较大、TURP后PSA水平较低的低风险或中风险患者可考虑保守治疗。因此,TURP后PSA的水平可能有助于风险分层和保守治疗患者的选择。
原始出处:
Chun-Te Wu , Yun-Ching Huang , Wen-Cheng Chen et al. The Predictive Role of Prostate-Specific Antigen Changes Following Transurethral Resection of the Prostate for Patients with Localized Prostate Cancer. Cancers (Basel). Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#尿道#
37
#切除术#
38
#局部前列腺癌#
39
#前列腺切除#
27
#ERS#
33
#前列腺特异性抗原#
42
#特异性抗原#
34
#特异性#
32
#局部#
33
#抗原#
29