Nature Neuroscience:清华大学时松海团队揭示细胞代谢方式及相关产物调控大脑新皮层发育的关键作用机制
2022-06-28 小柯生命 小柯生命
北京时间2022年6月20日晚23时,清华大学时松海课题组在Nature Neuroscience杂志在线发表了题为“Metabolic lactate production coordi
北京时间2022年6月20日晚23时,清华大学时松海课题组在Nature Neuroscience杂志在线发表了题为“Metabolic lactate production coordinates vasculature development and progenitor behavior in the developing mouse neocortex”(乳酸代谢调控小鼠大脑新皮层血管生长和神经前体细胞行为)的研究论文。
该研究揭示了大脑新皮层发育过程中的早期增殖型放射状胶质前体细胞(Radial glia progenitor,RGP)具有更强的糖酵解代谢能力并大量合成和分泌乳酸,进而调节血管生长及其自身增殖分裂特性。
大脑新皮层是神经系统的最高级中枢,理解大脑新皮层的发育组装及工作机制是脑科学乃至整个自然科学的终极目标之一。研究大脑新皮层的发育及其调控机制有助于更好地理解其细胞组成和结构特性,进而推动生理功能和运行工作机制的认知,同时对相关疾病的诊断治疗有着至关重要的意义。大脑新皮层是进化的末期产物,其发育是一个高度复杂且受到多种因素的共同调节的生物学过程,这也为系统性研究其内在机制带来了诸多挑战。为此该研究从细胞最为基本特征—细胞代谢的角度出发,揭示了细胞代谢方式及相关产物在调控大脑新皮层发育过程中的关键作用和机制,为更好的理解大脑皮层发育机制提供了重要的理论补充。
放射状胶质前体细胞(RGP)是大脑发育最为关键的一种神经前体细胞,其分裂产生大脑皮层几乎所有的神经元和胶质细胞。在小鼠发育早期(E10.5-E11.5),大脑新皮层中几乎没有血管生长,此时RGP以对称分裂进行增殖。伴随着血管的生长,RGP也随之改变其分裂方式,以不对称分裂进行神经细胞产生。基于单细胞代谢状态分析,该研究首先发现大脑新皮层发育过程中,随着RGP谱系发生过程的进行,RGP及其子代细胞具有不同的代谢状态,并呈现出不同的代谢特征。在此基础上,结合基因表达分析、细胞代谢类型分析以及碳代谢流分析多方面研究,进一步发现进行对称分裂的增殖型RGP具有更强的糖酵解代谢能力,并大量合成和分泌乳酸,而进行不对称分裂的分化型RGP具有更强的氧化磷酸化代谢能力,并积累高浓度的乙酰辅酶A。
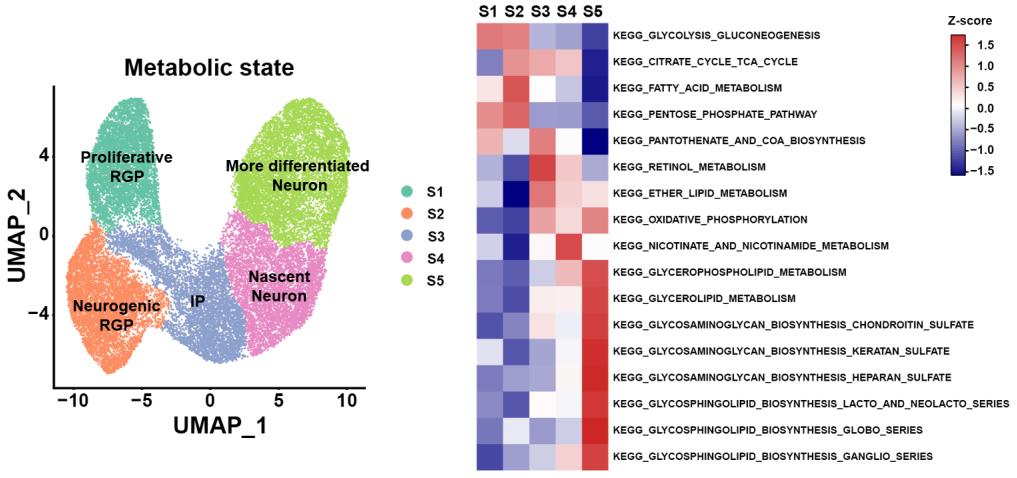
图1: 单细胞代谢状态分析揭示神经细胞代谢特征
为深入探讨细胞代谢方式与大脑新皮层发育的相互关系,研究者考察了具有强糖酵解代谢能力的增殖型RGP对早期大脑新皮层发育的影响,发现当抑制增殖型RGP的乳酸合成或分泌,导致大脑新皮层中乳酸浓度降低,血管生长出现缺陷。进一步分析发现,乳酸可以通过调节趋化因子配体CXCL1的表达来调节血管内皮细胞的迁移和增殖。此外,研究者发现抑制增殖型RGP的乳酸合成代谢会系统性改变其基因表达谱并重塑细胞代谢方式,导致RGP过早分化。为探讨这一内在机制,研究者发现与分化型RGP相比,增殖型RGP呈现出更长的线粒体形态,抑制或阻断乳酸合成或分泌都会导致线粒体长度大幅度缩短,进而导致RGP分化。该结果表明增殖型RGP通过加强乳酸合成来影响线粒体形态,进而保持其对称分裂增殖特性。
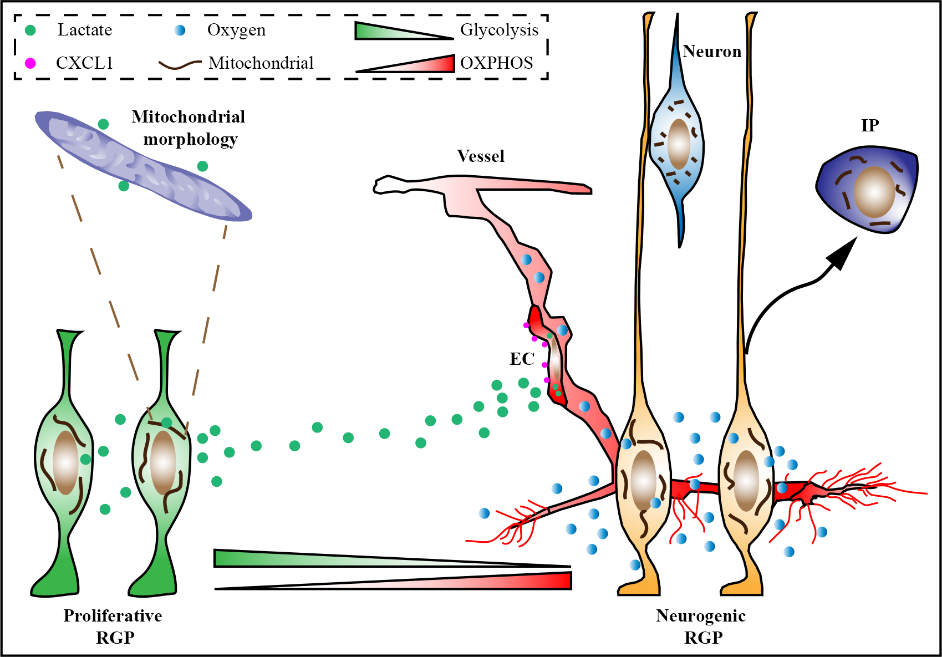
图2: 乳酸合成代谢调控早期大脑新皮层发育
清华大学生命科学学院时松海教授为本文通讯作者,清华大学生命科学学院2017级博士董晓翔为本文第一作者。清华大学生命科学学院张强强博士和马健博士、清华大学生命科学学院博士研究生于翔宇和王玎,以及美国达特茅斯学院本科生马嘉明为本文共同作者。该研究得到了清华大学实验动物中心和生物医学测试中心的大力协助和支持。
该研究获得了国家自然科学基金委创新群体基金、国家科技部脑科学与类脑研究基金、北京市教育委员会卓越青年科学家计划、北京市科技委员会科技计划、北京生物结构前沿研究中心、生命科学联合中心和北京脑科学与类脑研究中心的资助。
原始出处:
Dong, X., Zhang, Q., Yu, X. et al. Metabolic lactate production coordinates vasculature development and progenitor behavior in the developing mouse neocortex. Nat Neurosci (2022). https://doi.org/10.1038/s41593-022-01093-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
33
#发育#
26
#ROS#
32
#SCIE#
37
#清华#
45
#细胞代谢#
32