JU:根治性前列腺癌切除术后切缘为良性腺体组织是否与生化复发相关
2021-09-15 泌尿小王 MedSci原创
理论上讲,RP后血清前列腺特异性抗原(PSA)检测不出来。然而,研究发现,部分患者在接受明确RP治疗后且没有肿瘤复发,仍能检测到PSA,手术切缘的良性腺体组织是否与PSA和/或术后的BCR有关
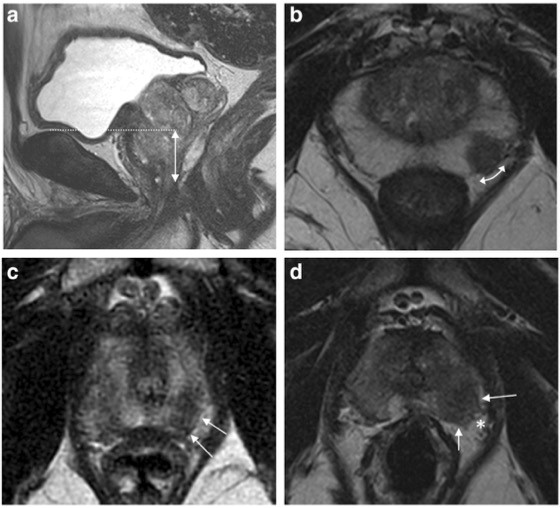
理论上讲,根治性前列腺癌切除术(RP)后血清前列腺特异性抗原(PSA)检测不出来。然而,研究发现,16.4%的患者在接受明确RP治疗后且没有肿瘤复发,仍能检测到PSA;而对于孤立性膀胱癌,接受膀胱前列腺切除术后可检测到PSA,这一比例高达12%;手术切缘的良性腺体组织(BGM)是否与PSA和/或RP后的生化复发(BCR)相关仍然有待研究。
最近,《The Journal of Urology》发表了一篇研究对该问题进行了研究而结果提示RP时BGM的存在与MSM、PSA检测、BCR或PSA检测后进展的风险增加无关。
方法
2004-2018年接受RP的患者,总计1082名。
纳入标准:
(1)纳入研究的患者必须在RP后6个月内有PSA <0.03 ng/ml的记录
(2)术后两次的PSA检测需要在术后8周内完成检测,术后至少随访6个月。
排除标准:
(1)在诊断时患有临床T4、N1或M1疾病的男性或病理性N1疾病的男性被排除在外
(2)在RP之前接受新辅助治疗的患者被排除在外
(3)在RP后6个月内开始辅助治疗的患者
BCR定义为RP后至少8周连续2次PSA ≥ 0.2 ng/ml。
BGM被定义为手术切缘为良性前列腺组织。
结果
共有1082名男性因局部前列腺癌伴BGM接受RP治疗,249例(23%)标本中存在BGM。
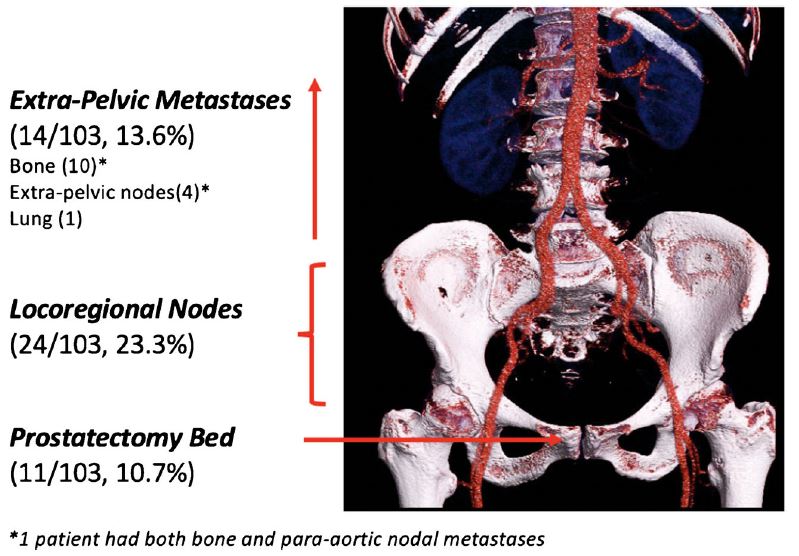
年轻、双侧神经保留手术和机器人入路与BGM相关,而手术边缘恶性肿瘤(MSM)不相关。在RP术后7年,29%的患者检测到PSA, 11%的患者有BCR。
在达到可检测PSA的男性亚组中,79%的人在7年内有进展。在多变量Cox比例风险回归分析中,BGM状态与可检测PSA、BCR和/或从可检测PSA进展到BCR或挽救性治疗无关。
结论
RP术后残余的良性腺体组织与PSA和BCR不相关
文献来源
Greenberg SA, Washington SL 3rd, Lonergan P, et al. Residual Benign Prostate Glandular Tissue after Radical Prostatectomy is Not Associated with the Development of Detectable Postoperative Serum Prostate Specific Antigen. J Urol. 2021 Sep;206(3):706-714. doi: 10.1097/JU.0000000000001793. Epub 2021 Apr 27. PMID: 33905262.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#切除术#
28
#生化复发#
37
#根治#
30
这个活动即可以领略到各科的新知识新动向,又可以参加抽奖,学习中伴随着抽奖有趣
61
学习
55
前列腺癌相关研究,学习了,谢谢梅斯
51
学习
45