Cardiovasc Diabetol:真实世界既往无心梗/卒中病史人群中冠状动脉疾病合并2型糖尿病的发生率
2021-11-26 Nebula MedSci原创
THEMIS样人群CAD-T2DM的患病率估计为1.50/1000人,约占没有心肌梗死/卒中病史的CAD-T2DM患者的四分之一,而THEMIS-PCI样人群CAD-T2DM的患病率为0.27/100
冠状动脉疾病 (CAD) 是导致死亡和发病的主要原因之一。2 型糖尿病 (T2DM) 是众所周知的 CAD、心肌梗塞 (MI) 和/或卒中的危险因素。THEMIS随机试验对比了替格瑞洛联合阿司匹林与安慰剂联合阿司匹林治疗既往无心肌梗死 或卒中的合并 2 型糖尿病的稳定型冠状动脉疾病 (CAD-T2DM) 患者的效果和安全性。
本研究旨在量化真实世界环境中,既往没有心肌梗死或卒中病史人群中CAD-T2DM患者人群的规模(更进一步是具有类似 THEMIS 纳入标准的人群[THEMIS 样和 THEMIS-PCI 样人群]),以及其在当前临床实践背景下主要预后的风险。
一项为期 2 年的随访队列研究纳入了 2014 年 1 月 1 日前收录在SNDS法国全国索赔数据库中的所有无心肌梗死/卒中病史的CAD-T2DM患者。THEMIS样患者人群为≥50岁的符合THEMIS纳入及排除标准的患者。采用累积发生率估算临床预后的发生率(包括心肌梗死、缺血性卒中、大出血等)。
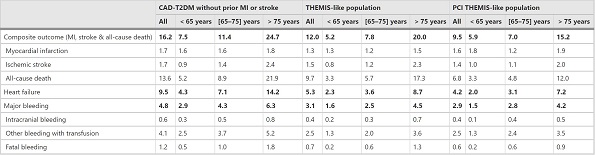
各种预后的两年累积发生率
在约 5000 万成年人中,无心肌梗死/卒中病史、THEMIS 样和 THEMIS-PCI 样人群的CAD-T2DM患病率分别为 6.04/1000人、1.50/1000人 和 0.27/1000人,平均年龄分布是72.7岁、72.3岁和70.9岁;THEMIS 样和 THEMIS-PCI 样人群的合并症和糖尿病并发症均更少。无心肌梗死/卒中病史、THEMIS 样和THEMIS-PCI 样CAD-T2DM患者的两年心肌梗死累积发生率分别是1.7%、1.3%和1.6%,两年卒中累积发生率分别是1.7%、1.5%和1.4%,大出血的分别是4.8%、3.1%和2.9%,全因死亡率分别是13.6%、9.7%和6.8%;复合终点(心梗、卒中和全因死亡)的分别是16.2%、12.0%和9.5%。
综上,THEMIS样人群CAD-T2DM的患病率估计为1.50/1000人,约占没有心肌梗死/卒中病史的CAD-T2DM患者的四分之一,而THEMIS-PCI样人群CAD-T2DM的患病率为0.27/1000人。
原始出处:
Blin, P., Darmon, P., Henry, P. et al. Patients with stable coronary artery disease and type 2 diabetes but without prior myocardial infarction or stroke and THEMIS-like patients: real-world prevalence and risk of major outcomes from the SNDS French nationwide claims database. Cardiovasc Diabetol 20, 229 (2021). https://doi.org/10.1186/s12933-021-01416-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
31
#BET#
37
#ASC#
35
#发生率#
33
#冠状动脉疾病#
0
#真实世界#
30