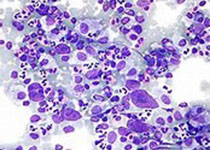
NEJM:高风险、成熟的B细胞非霍奇金淋巴瘤儿童利妥昔单抗疗效分析
2020-06-04 MedSci原创 MedSci原创
在标准LMB化疗中加入利妥昔单抗可显著延长高级别、高风险、成熟B细胞非霍奇金淋巴瘤的儿童和青少年的无事件生存期和总体生存期,并与较高的低丙种球蛋白血症发生率相关,并且伴有更高的感染发作几率。
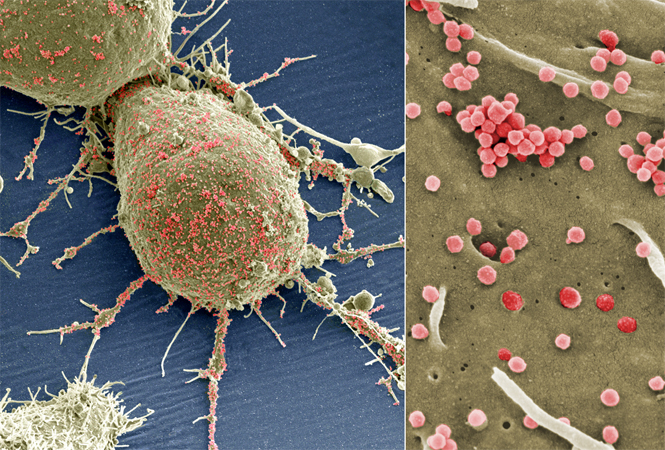
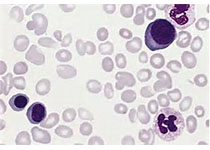
将利妥昔单抗添加到化疗方案中可延长B细胞癌成年患者的生存期。关于其对高度、成熟的B细胞非霍奇金淋巴瘤儿童的疗效和安全性的数据十分有限。
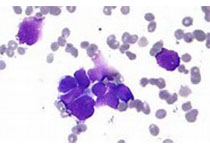
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项开放标签、国际、随机、3期临床试验,研究对象为18岁以下的高危成熟B细胞非霍奇金淋巴瘤(伴有乳酸脱氢酶水平升高的III期或IV期)或急性白血病患者,以比较标准的淋巴瘤马林斯B(LMB)化疗加入6个疗程的利妥昔单抗与单独的标准LMB化疗。该研究的主要终点是无事件生存率。研究人员还评估了总生存期和毒性效应。
该研究的分析基于328例接受随机分组的患者(每组164例);85.7%的患者有Burkitt's淋巴瘤。中位随访时间为39.9个月。利妥昔单抗+化疗组中有10例患者发生了终点事件,化疗组中有28例患者观察到终点事件。利妥昔单抗+化疗组3年无事件生存率为93.9%(95%置信区间[CI]为89.1至96.7),化疗组为82.3%(95%CI为75.7至87.5)(原发难治性疾病或首次出现进展、反应后复发、任何原因导致的死亡或第二次癌症的风险比为0.32;95%CI为0.15至0.66;单侧P=0.00096)。利妥昔单抗+化疗组中有8例患者死亡(与疾病相关的死亡4例,与治疗相关的死亡3例,与第二种癌症相关的死亡1例),化疗组20例患者死亡(与疾病相关的死亡17例,与治疗相关的死亡3例)(风险比为0.36;95%CI为0.16至0.82)。前期治疗后,利妥昔单抗+化疗组4级或更高级别的急性不良事件发生率为33.3%,化疗组为24.2%(P=0.07);事件主要与发热性中性粒细胞减少和感染有关。进入试验1年后,利妥昔单抗+化疗组低IgG水平的患者约为化疗组的两倍。
由此可见,在标准LMB化疗中加入利妥昔单抗可显著延长高级别、高风险、成熟B细胞非霍奇金淋巴瘤的儿童和青少年的无事件生存期和总体生存期,并与较高的低丙种球蛋白血症发生率相关,并且伴有更高的感染发作几率。
原始出处:
Véronique Minard-Colin.et al.Rituximab for High-Risk, Mature B-Cell Non-Hodgkin’s Lymphoma in Children.NEJM.2020.https://www.nejm.org/doi/full/10.1056/NEJMoa1915315
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效分析#
28
#高风险#
32
#利妥昔#
29
#B细胞#
31
#B细胞非霍奇金淋巴瘤#
40
谢谢梅斯提供这么好的信息,学到很多
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
48