Eur Heart J:选择性冠脉重建相比药物治疗可进一步改善冠心病患者预后
2021-06-06 Nebula MedSci原创
对于稳定性冠状动脉疾病患者,与单纯药物治疗相比,选择性冠状动脉重建联合药物治疗可降低心源性死亡率
冠状动脉疾病是全球50岁以上人群最常见的疾病。除了常规药物治疗之外,冠状动脉重建也是冠状动脉疾病患者常用的治疗方式。
但选择性冠状动脉重建联合药物治疗在稳定性的冠状动脉疾病患者管理中的价值仍存有争议。本研究旨在回顾性分析在冠状动脉疾病中对比单纯药物治疗和选择性冠状动脉重建联合药物治疗的疗效和安全性。
从研究开始到2020年11月,研究人员在MEDLINE、EMBASE、谷歌学术和其他数据库中检索了比较临床稳定性冠状动脉疾病患者血管重建与单纯药物治疗的随机试验。使用随机效应模型,以95%置信区间(CI)的率比(RRs)检测治疗效果。预定的主要终点是心源性死亡率。次要终点是自发性心肌梗死(MI)及其与心源性死亡率的相关性,以及全因死亡率、任何心肌梗死和卒中。提取最长随访数据。
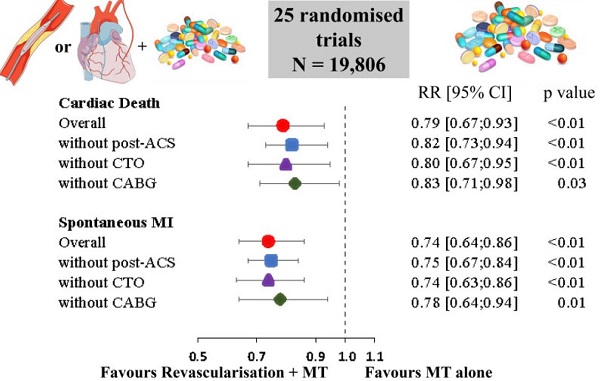
心源性死亡和自发性心肌梗死的风险比
总体上,本次分析纳入了25项试验,共包含19806位患者(10023位随机接受血运重建联合药物治疗,9783位单纯药物治疗)。与单纯药物治疗相比,血运重建降低了心源性死亡风险[RR 0.79 (0.67-0.93), P<0.01]和自发性心肌梗死风险[RR 0.74 (0.64-0.86), P<0.01]。
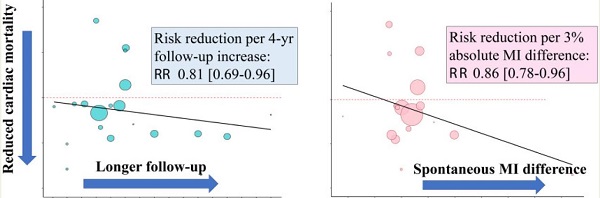
心源性死亡和自发性心肌梗死的发生率随时间的变化
荟萃回归分析显示,与单纯药物治疗相比,血管重建后心源性死亡风险降低与随访时间(4年随访RR: 0.81 (0.69-0.96), P=0.008)、自发心肌梗死绝对差异(P=0.01)和基线时多血管疾病百分比(P=0.004)呈线性相关。试验序列分析和敏感性分析证实了心源性死亡率结果的可靠性。
此外,各治疗方案间的全因死亡率[RR 0.94 (0.87-1.01),P=0.11]、任何心肌梗死(P=0.14)和卒中风险(P=0.30)均无显著差异。
综上所述,对于稳定性冠状动脉疾病患者,与单纯药物治疗相比,选择性冠状动脉重建联合药物治疗可降低心源性死亡率。而且随着随访时间的延长,血运重建后心脏生存获益改善,并与较少的自发性心肌梗死相关。
原始出处:
Navarese Eliano P,Lansky Alexandra J,Kereiakes Dean J et al. Cardiac mortality in patients randomised to elective coronary revascularisation plus medical therapy or medical therapy alone: a systematic review and meta-analysis.[J] .Eur Heart J, 2021, undefined: undefined. https://doi.org/10.1093/eurheartj/ehab246
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者预后#
35
#选择性#
39
#ART#
36
#冠心病患者#
42
#HEART#
37