腓骨肌皮瓣修复6岁儿童创伤性口腔颌面部缺损:1例报告及文献复习
2019-09-19 江灿洋 黄立 李军 中国口腔颌面外科杂志
女,6岁,于入院前12d,左侧面部不慎被电风扇切割,导致颜面部大面积缺损,大量出血,同时伴右上肢手掌丢失。发现患儿时其呈昏迷状态,将其急诊送于当地医院行“面部外伤清创缝合术+右上肢清创术+气管切开术”;术后予以抗感染、补液、止血、营养支持、镇痛等对症治疗,全身病情稳定后转诊于我院。经查体,以“左侧颌面部外伤性软、硬组织缺损”收入院。
口腔颌面部缺损往往由外伤、肿瘤、先天畸形和各类瘢痕切除后造成,影响患者的美观和功能。随着医学技术的发展,显微血管化组织瓣修复技术已成为一种重要的治疗手段。通过查阅文献,目前明确有关报道游离血管化腓骨肌瓣用于儿童颌骨缺损修复的病例中,国内最小年龄为10岁,国外为8个月;而同时修复软、硬组织缺损的病例非常罕见。与成人相比,处于生长发育期儿童的颌面部缺损重建,不仅需要考虑患儿的功能和外观,还需重视其心理健康发展。本文报告1例罕见的6岁儿童因切割伤导致口腔颌面部大面积软、硬组织缺损病例,并对相关文献进行复习及讨论。
1.病例报告
女,6岁,于入院前12d,左侧面部不慎被电风扇切割,导致颜面部大面积缺损,大量出血,同时伴右上肢手掌丢失。发现患儿时其呈昏迷状态,将其急诊送于当地医院行“面部外伤清创缝合术+右上肢清创术+气管切开术”;术后予以抗感染、补液、止血、营养支持、镇痛等对症治疗,全身病情稳定后转诊于我院。经查体,以“左侧颌面部外伤性软、硬组织缺损”收入院。
专科检查:左侧颜面部肿胀明显,见软组织裂伤清创缝合术后瘢痕,局部创口处见唾液储留;左侧面下1/3见大面积软组织和部分下颌骨、上颌部分牙槽骨缺损,创面范围约7 cm×5 cm,创缘不规则,唾液外溢,见肉芽组织生成覆盖。左侧乳牙列无咬合,右侧乳牙列深覆盖。51、61、62、63、71、72、73、74、8缺失,舌体活动自如,伸舌居中(图1A)。

图1 术前。A.缺损外观;B.3D-CT影像;C.RP模型
术前准备:血常规、肝功能、肾功能、电解质、凝血全套等检验学检查,头颅CT平扫+三维重建(图1B),颌骨RP模型(图1C),下肢血管CTA等,各项术前检查均未见明显全麻手术禁忌证。手术方案:左侧游离血管化腓骨肌皮瓣制备,修复左侧下颌骨、口底、面部软、硬组织重度缺损+血管吻合术+左侧大腿内侧取皮转移小腿植皮术(图2)。

图2 术中所见。A.瘢痕松解后缺损观;B.设计的腓骨肌皮瓣;C.颌面部缺损重建后
2.结果
术后给予抗感染、抗痉挛、活血等对症治疗,腓骨肌皮瓣血运良好(图3A),涎瘘症状消失。术后2周拔除气管套管,复查颌骨CT平扫+三维重建(图3B),口唇完全闭合,进流质饮食、言语流利。出院时小腿植皮区基本愈合。术后3个月复诊,患儿能够自由行走,各切口愈合良好,面部形态满意。曲面体层片显示,移植的腓骨肌皮瓣与下颌骨相融合,形态良好(图3C)。
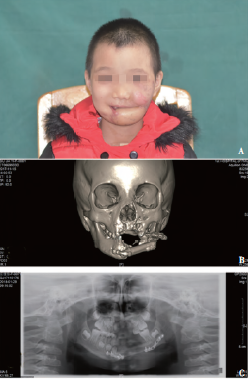
图3 术后图片。A.修复术后外观;B.术后3D-CT;C.术后3个月曲面体层片
3.讨论
通过大样本数据收集分析,Michael等报道儿童头颈部组织缺损的原因有先天畸形(31.9%)、肿瘤切除术后(51.1%)、复合型(12.8%)、烧伤(2.1%)、创伤(2.1%)等,其中创伤所占比例小,而同时伴有软组织和骨组织缺损的病例更为罕见。相比于成人,儿童的颌骨处于生长改建期,颌面部组织缺损特别是骨组织缺损会导致颌骨发育不足、咬合关系紊乱、面部不对称等继发性畸形;随着儿童生长发育,患儿不仅存在生理创伤,还可能有心理障碍,影响其生活质量和社会交往。
先天性畸形或肿瘤切除术后导致的缺损可以同期进行修复重建,而创伤导致的颌面部缺损常伴有严重感染、瘢痕形成、创口形状不规则甚至出现失血性休克等,需二期手术治疗。对于软组织缺损,临床上可采用游离血管化前臂皮瓣、股前外侧皮瓣、侧胸皮瓣、腹直肌皮瓣等修复;而骨组织缺损则可采用肋骨、肩胛骨、腓骨、髂骨等自体骨修复;对于同时伴有软、硬组织缺损的颌面部缺损,目前采用的修复技术有牵张成骨术、游离血管化腓骨肌皮瓣、肩胛骨肌皮瓣、髂骨肌皮瓣和组织工程技术等。
本文报告的病例中,制备一块长7 cm的游离血管化腓骨附一块大小约8 cm×7 cm的皮岛修复巨大颌面部缺损。因小腿创口无法直接关闭,遂于同侧大腿内侧制取中厚层皮片,移植于小腿创面,术后未出现严重并发症。小儿腓骨较细且周围附着组织较为疏松且脆弱,在制取过程中需更加仔细解剖和保护血管神经,避免损伤骨膜和造成医源性腓骨骨折而影响血运。腓骨肌瓣具有足够的厚层皮质骨和骨长度,必要时还可同时制备充足的软组织瓣,临床上适用于修复颌面部大面积软、硬组织缺损。
据相关文献报道,儿童颌骨缺损特别是下颌骨缺损也可采用游离血管化腓骨瓣修复,恢复颌骨的长度及形态,目前年龄尚无统一规定。由于儿童手术耐受能力差,术前需要全面考虑供区和受区条件、可能发生的并发症,尽量缩短手术时间。儿童的血管管径细小,要求手术医师具有高水平的显微缝合技术,在直视操作下吻合血管;术后积极抗血栓、抗痉挛和抗感染治疗,密切观察皮瓣的血运状况,保证手术成功。此病例术中探见面动脉管腔如针孔样大小,腓动、静脉分别与面动脉和颈外静脉吻合。
周铜等认为,儿童皮下组织疏松,术后水肿较成人更明显,在设计皮瓣时候,尤其要注意皮瓣的充分回流,静脉、动脉比为3∶2或2∶1。Melissa等认为,如果下颌骨生长中心不受干扰,移植的腓骨能适应下颌骨生长而改建,但不影响咬合,并且腓骨的长度和高度都有明显的生长和改建。本文报告的病例还需长期随访观察,而且计划多次手术,进行口腔颌面部整复,为患儿健康成长创造条件。
原始出处:
江灿洋,黄立,李军,邱宇,高炳菊,林李嵩.腓骨肌皮瓣修复6岁儿童创伤性口腔颌面部缺损:1例报告及文献复习[J].中国口腔颌面外科杂志,2018(05):475-477.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#创伤性#
47
#腓骨肌#
34
#口腔颌面部#
35
#肌皮瓣#
29
#创伤#
21
#皮瓣#
35