B细胞受体(BCR)信号转导和T细胞相互作用在慢性淋巴细胞白血病(CLL)的发病机制和病程进展中起着关键作用。CLL细胞可以利用microRNAs(MiRNAs)及其靶基因来调节淋巴结壁龛内的微环境相互作用。
为了确定miRNA在CLL微环境中的表达变化,研究人员通过比较CXCR4/CD5克隆内细胞亚群(CXCR4dimCD5bright与CXCR4brightCD5dim细胞),对短链非编码RNA进行了复杂的图谱分析。

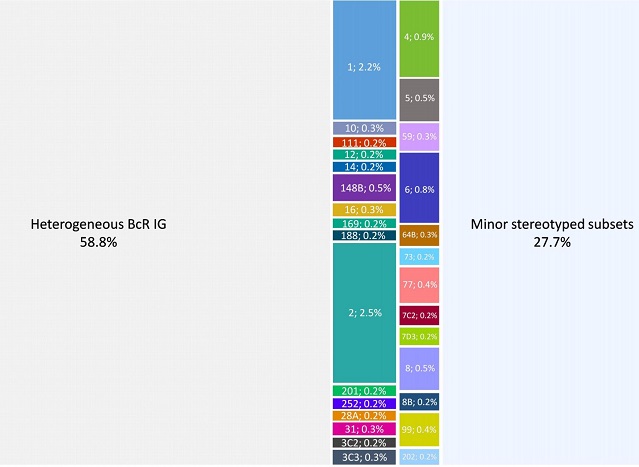
结果发现了数十个差异性表达的miRNAs,其中几个已被证明了参与调节BCR信号的miRNAs(miR-155、miR-150和miR-22)。值得注意的是,miR-29家族的全部成员(miR-29a、miR-29b、miR-29c)都在免疫微环境中持续下调,且miR-29(a/b/c)水平的降低与CLL细胞对BCR阻断的相对反应性增强以及CLL患者的总生存期显著缩短有关。
miR-29的表达水平与总生存期的关系
此外,研究人员还发现肿瘤坏死因子受体相关因子4(TRAF4)是miR-29s的一个新的直接靶点,高TRAF4水平可增加CLL对CD40激活和下游NFkB信号的反应性。在CLL中,BCR通过MYC抑制miR-29的表达,同时允许TRAF4上调和CD40-NFkB信号增强。该调控环路可被“BCR抑制剂”(BTK抑制剂依鲁替尼或PI3K抑制剂idelalisib)破坏。
总结模式图
综上所述,该研究首次展示了CLL微环境中激活CD40信号/T细胞相互作用的miRNA依赖性机制,并描述了一个受BCR活性调控的新的miR-29-TRAF4-CD40信号轴。
原始出处:
Sharma Sonali,Pavlasova Gabriela Mladonicka,Seda Vaclav et al. miR-29 Modulates CD40 Signaling in Chronic Lymphocytic Leukemia by Targeting TRAF4: an Axis Affected by BCR inhibitors. Blood, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TRA#
21
#CD4#
32
#miR#
25
#TRAF4#
29