有时候在想,明明 CT 看出血那么清楚明白,为什么还要用核磁这么烧脑的影像工具呢?
直到有一天,一个病人出现了,CT 上的出血如此清晰,如此简单,如此小 case,哎慢着慢着,这个出血好奇怪……不像是高血压性脑出血……难道有畸形……还是做个核磁吧……
那么,核磁上血管畸形导致的脑出血又有什么特点呢?
先来看看各种血管畸形的示意图
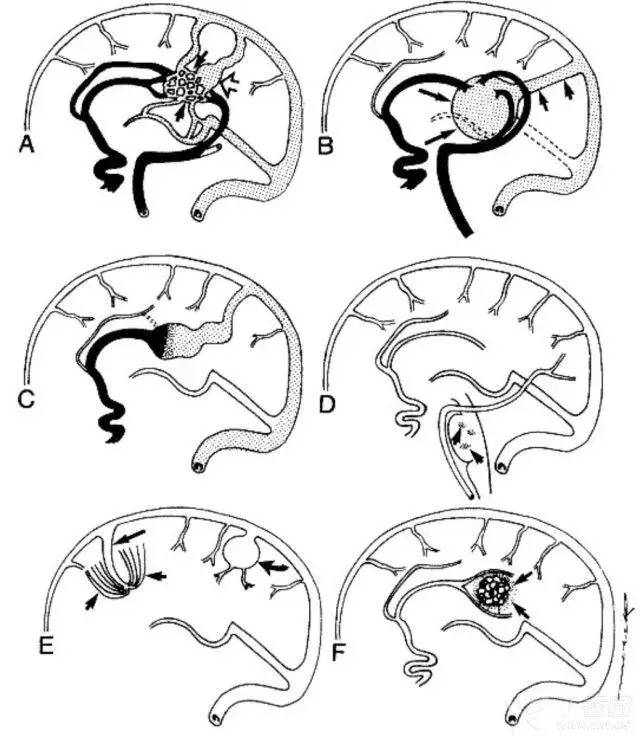 A:动静脉畸形伴丛状小巢(小箭):黑线示供血动脉,小点区为引流静脉,空白箭头示饮酒静脉区的静脉曲张;
A:动静脉畸形伴丛状小巢(小箭):黑线示供血动脉,小点区为引流静脉,空白箭头示饮酒静脉区的静脉曲张;
B:大脑大静脉畸形:巨大的大脑大静脉(大箭)通过永存镰状窦引流(小箭);
C:软脑膜动静脉瘘:可见不规则的动脉(实黑线)引流入一扩张的皮层静脉(小点状区);
D:脑桥血管畸形;
E:静脉畸形:小箭示一伞状扩张的髓质静脉团,大箭示扩张的引流静脉;弯箭示另一类型的静脉畸形;
F:海绵状血管瘤:箭头所示为含铁血黄素沉积。
动静脉畸形(AVM)
AVM 是颅内血管畸形中最多见的,病变由一团紧密连接在一起的粗细不均匀的异常血管组成。多发于大脑半球,以大脑中动脉供血区最为多见。
CT 上 AVM 常为混杂密度影,供血及引流血管呈迂曲的条样等密度或高密度,病灶内可见条样或点状钙化,边界不清。
约 2/3 患者可发生出血,其出血表现与高血压性脑出血相似。
当脑出血患者表现为以下几种情况时,要考虑 AVM:
(1)血肿位于大脑表浅部位;
(2)CT 平扫时血肿中可能有相对低密度的畸形血管,或者钙化的血管影;
(3)MR 检查时显示血肿内或附近有血管流空影,T1 及 T2 像上均为无信号暗区;
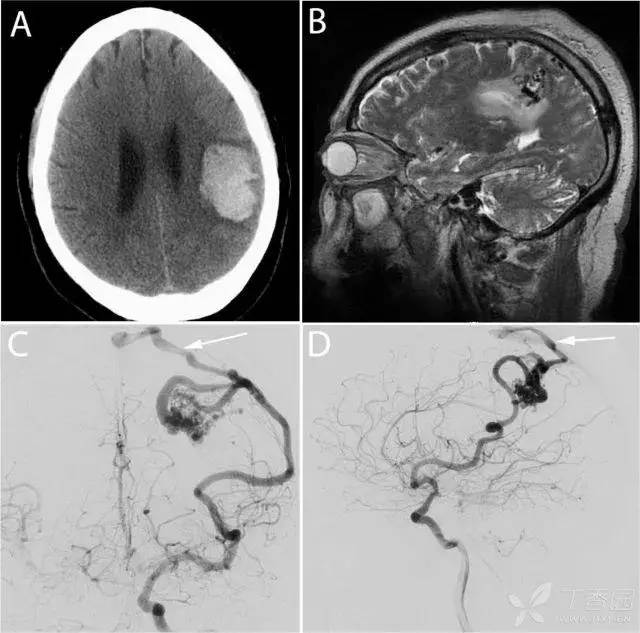
72 岁男性,左侧额顶叶 AVM 伴出血。A:平扫 CT 示出血灶,病灶内密度不均匀;B:左侧顶叶可见血管流空影,提示 AVM;C-D:DSA 显示 AVM,供血动脉为左侧 MCA,引流静脉为皮层静脉 [1]。
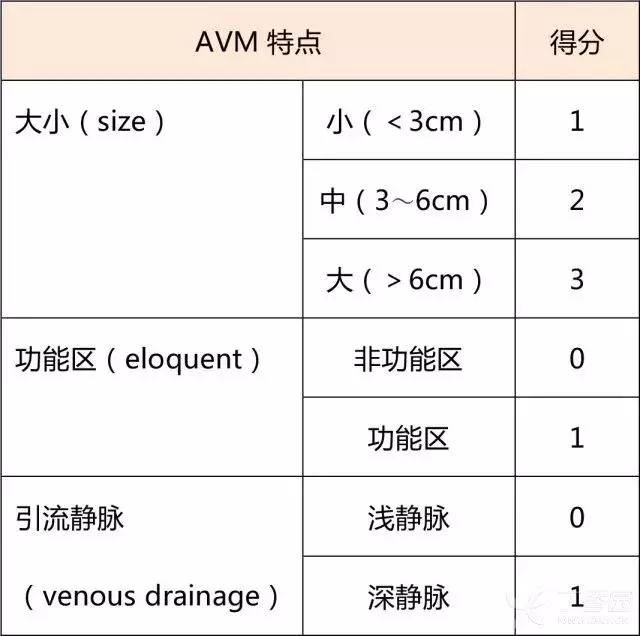
以下图表为 Spetzler-Martin AVM 分级 [2]:
除了动静脉畸形,海绵状血管瘤(CMs)、发育性静脉异常(DVAs)等在核磁上怎么看呢?留给大家思考吧,留言区一较高下吧!!!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
41
#期刊论坛##学习#
58
不错的文章
45
#磁共振#
38