【所属科室】
普外科
【基本资料】
男,30岁
【主诉】
体检B超发现盆腔实性包块,无症状
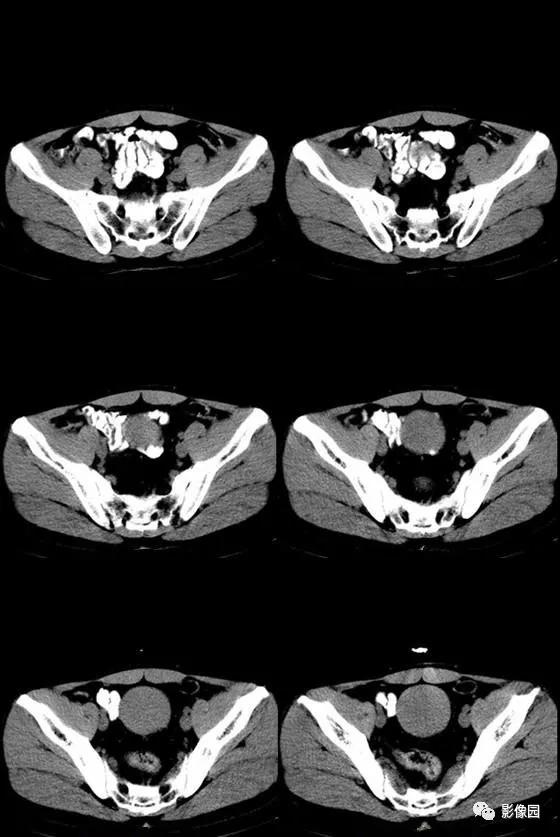
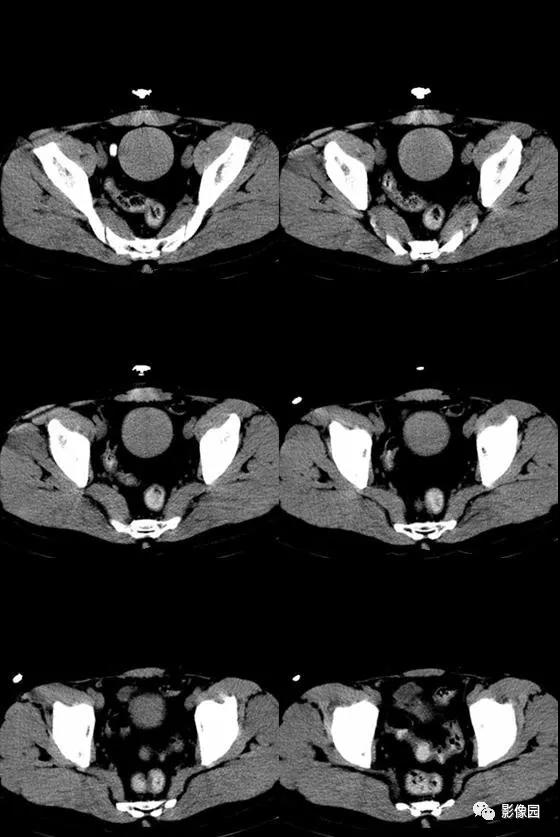
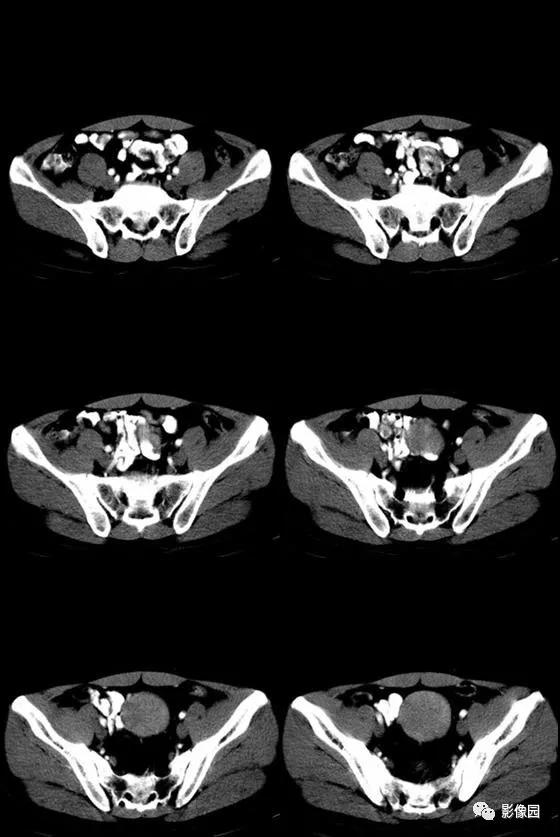
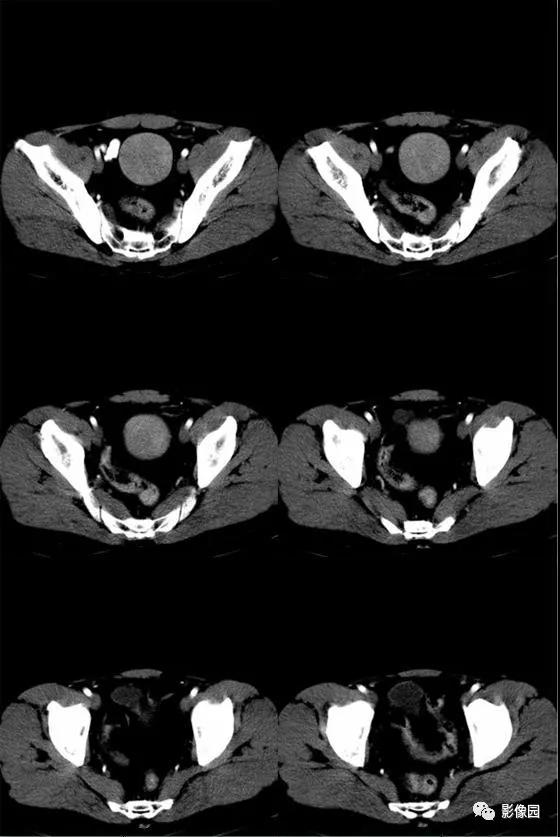
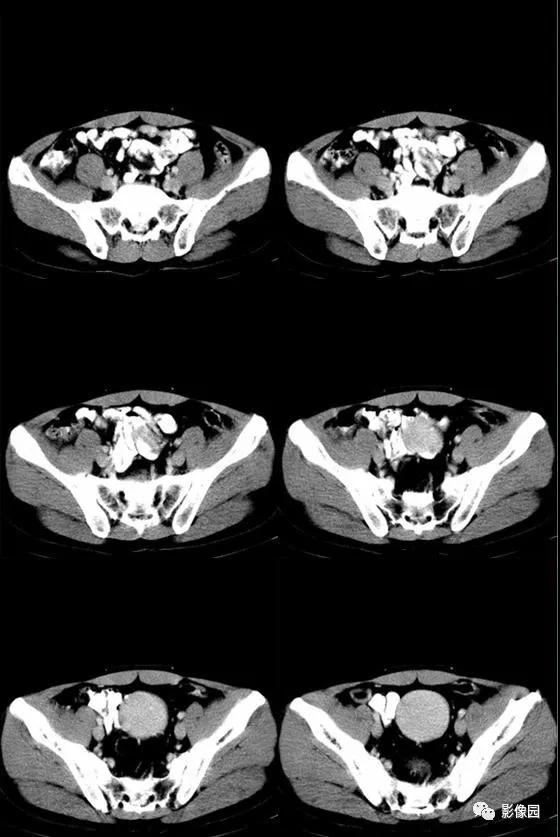
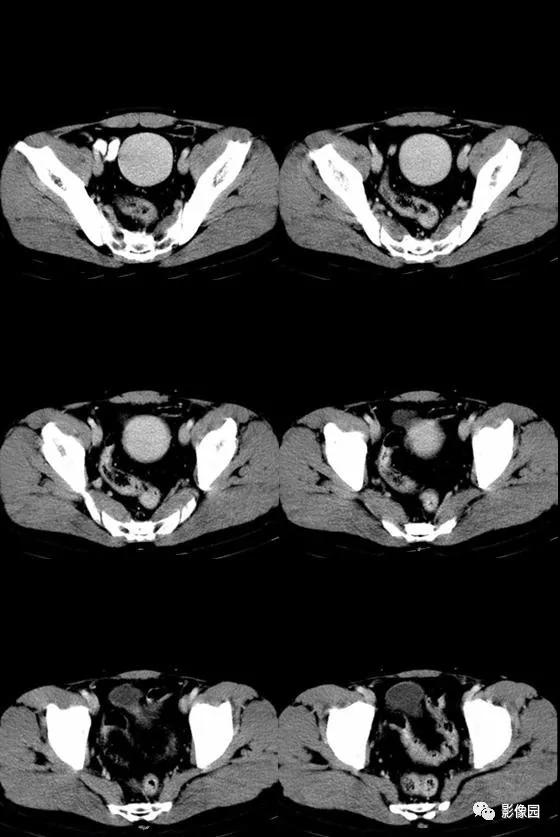
【影像图片】
【讨论】
评论:盆腔内见以类圆形软组织密度影,边缘清楚,密度均匀,周围肠腔稍受压变形,增强后病灶呈均匀性强化;盆腔内未见明显肿大淋巴结;余未见明显异常。间质瘤?
【病理结果】
病理结果:副脾
【病例小结】
副脾是一种并不少见的先天性变异,是存在于正常脾脏以外,与正常脾脏结构相似、功能相同的组织,其发生可能因胚胎期始基芽融合不全或异位脾芽形成,或部分脾组织脱落主脾块发育而成,并具有单独的动、静脉。
副脾多位于脾门、脾蒂或脾尾部位,少数出现于脾胃、脾结肠韧带、大网膜及其他部位。本例副脾位于盆腔内,较为少见,易误诊为肠系膜或腹膜来源的病变。如果全腹部、盆腔同时行平扫并增强扫描的话,通过对比观察正常脾脏的强化方式、程度,并测量CT值变化情况,不失为一个鉴别的好办法。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#包块#
51
#体检#
24
#无症状#
18
#B超#
32